Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Antidepressant's Unusual Speed Explained
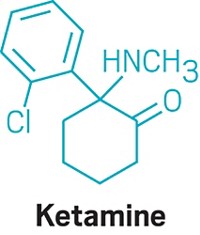
Neuroscience: Ketamine, which can overcome depression in hours, stimulates rapid synapse formation
by Sophie L. Rovner
August 19, 2010
| A version of this story appeared in
Volume 88, Issue 34

Unlike commercially available antidepressants, which require weeks or months to take effect, a single dose of ketamine can overcome depression in hours, a speed advantage that can spell the difference between life and death for suicidal patients. Researchers at Yale University School of Medicine have now discovered why the compound works so fast. Their findings illuminate the mechanisms underlying depression and also suggest new targets for its treatment.
Depression is believed to correlate with a reduction in the number of synapses, or connections between neurons, in the prefrontal cortex of the brain, notes Ronald S. Duman, who studies molecular psychiatry and pharmacology at Yale. Duman's team now reports that ketamine undoes this damage by increasing the number of these synapses in rats within 24 hours of administration, whereas traditional treatments do not (Science 2010, 329, 959).
The researchers determined that ketamine stimulates the mammalian target of rapamycin (mTOR) signaling cascade, which is involved in protein synthesis and synaptic modification in neurons. Ketamine activates this pathway by preventing the neurotransmitter glutamate from binding to the N-methyl-D-aspartate (NMDA) class of receptors on neurons.
"Together, these findings suggest that the rapid activation of mTOR-mediated signaling pathways may be an important and novel strategy for the rational design of fast-acting antidepressants," note John F. Cryan and Olivia F. O'Leary, neuropharmacologists at University College Cork, in Ireland, in a commentary about the work (Science 2010, 329, 913). They add that drugs that target this pathway would provide an alternative to the antidepressants currently on the market, nearly all of which function by boosting brain levels of neurotransmitters such as serotonin and norepinephrine.
Ketamine itself is unsuitable as a commercial antidepressant. At doses higher than required for the antidepressant effect, it serves as an anesthetic. It can induce hallucinations—hence its popularity as the street drug "Special K"—and it must be injected. Ketamine can be administered by a doctor, but this practice is inconvenient because the antidepressant effect of a dose wears off after about a week.
The pharmaceutical industry is now trying to develop safe, fast-acting antidepressants that can be given orally and can't be abused, says Duman.
One lead is Ro 25-6981, a compound originally developed by Roche. Duman's team showed that the compound acts on the mTOR pathway, just as ketamine does. But Ro 25-6981 might avoid ketamine's side effects because it activates only the NR2B subclass of NMDA receptors, Duman says.
Last month, Roche and the drug discovery and development firm Evotec announced the start of Phase II clinical studies of another potential rapidly acting antidepressant, a selective NR2B inhibitor called EVT 101.
Researchers hope that ketamine substitutes will preserve another impressive characteristic of the anesthetic—its ability to overcome depression in patients who don't respond to conventional treatments. For example, Carlos A. Zarate Jr., chief of experimental therapeutics at the National Institute of Mental Health in Bethesda, Md., and colleagues recently reported that a single injection of ketamine reduced depression after just 40 minutes in bipolar patients who had failed to obtain relief from other treatments (Arch. Gen. Psychiatry 2010, 67, 793). Furthermore, only 6% of participants responded to placebo, but 71% responded to ketamine.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter