Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Neuroscience
Designer drug detective work
Scientists at the National Institute on Drug Abuse race to understand the neurochemistry behind new street drugs
by Erika Gebel Berg, special to C&EN
July 11, 2016
| A version of this story appeared in
Volume 94, Issue 28

Sitting in his office in Baltimore, neurochemist Michael H. Baumann eagerly flipped through a spreadsheet. It listed hundreds of chemical names of suspected drugs seized by local, state, and federal law enforcement agencies over the past three years. “When police bust people with some white powder or a baggie full of pot-looking material, it gets sent to forensic laboratories, and they test what’s in it,” he says. All of that data gets dumped into a database cataloged by the Drug Enforcement Administration (DEA), and Baumann asks for a rundown of what’s been found.
That rundown provides Baumann, head of the Designer Drug Research Unit at the National Institute on Drug Abuse (NIDA), with a guide to the ever-changing world of designer drugs. As of December 2014, 541 new psychoactive substances—the preferred term for synthetic designer drugs—had been reported. And it’s reasonable to think that the number is higher now.

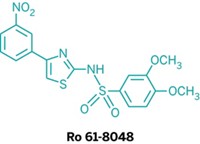
The drugs, often sold in stores and on the internet as innocuous-sounding “spice” or “bath salts,” are designed to mimic the physiological actions of well-characterized drugs such as marijuana, cocaine, ecstasy, LSD, and heroin, often via tweaks to the chemical structures of those compounds. “They are psychoactive drugs sold under false pretenses, often as household products,” Baumann says. “This is purely to skirt regulation.” Because these synthetic drugs are chemically distinct from controlled substances, they can be bought and sold in a quasi-legal market existing largely on the internet.
Baumann, along with four other scientists in the unit, examines the neurochemistry of these emerging psychoactive substances. The scientists focus mainly on compounds being sold in large volumes or linked to deaths. They try to determine what these molecules do in the brain to get users high. The team’s findings provide valuable information to forensic toxicologists and policy-makers involved with the growing problem of designer drugs.
Although some of these compounds are new to the illicit drug scene, they aren’t necessarily new molecules, Baumann says. “These drugs are being pulled from the scientific and patent literature.”
For example, John W. Huffman, professor emeritus of organic chemistry at Clemson University, has published studies on hundreds of chemicals that interact with cannabinoid receptors. This research has provided valuable insight into the brain’s endocannabinoid system, which affects appetite, mood, memory, and pain sensation. But rogue chemists have hijacked Huffman’s research, synthesizing vast quantities of the cannabinoids and selling them to people who want to get high—or more accurately, Baumann says, to people who want to get high on the sly. For example, a report published in September 2013 by the Office of National Drug Control Policy found that more than one-quarter of a sampling of Washington, D.C.-area men in the criminal justice system, such as parolees and probationers, tested positive for synthetic cannabinoids, despite the fact that many of those men had passed the standard drug test panel.
As with well-known drugs, these designer molecules can cause real harm. During the second half of 2013, a new street drug called 4,4’-dimethylaminorex (4,4’-DMAR) was responsible for a wave of 26 overdose deaths in Europe. To figure out what they were dealing with, European scientists contacted Baumann. A few months later, Baumann and his colleagues reported that 4,4’-DMAR had potent interactions with transporter proteins in the brain that normally take up neurotransmitters from the junctions, or synapses, between neurons and move them inside the cells (Drug Test. Anal. 2014, DOI: 10.1002/dta.1668). Specifically, 4,4’-DMAR caused these transporter proteins to release dopamine, norepinephrine, and serotonin into the synapses. This spike in neurotransmitter release likely contributes to increasing a user’s heart rate and body temperature, with deadly consequences. Baumann’s data helped authorities from several European countries outlaw 4,4’-DMAR.
Meanwhile, Baumann’s collaborator at Memorial Sloan Kettering Cancer Center, Gavril W. Pasternak, is about to initiate a program to study newly emerging opioid analogs. The opioid epidemic is already worrying drug enforcement in the U.S.: The New York Times reported that the opioid fentanyl, a powerful prescription painkiller that’s also synthesized in illegal laboratories, is now killing more people than heroin in some parts of New England. Acetyl fentanyl, a derivative with no legitimate uses, was responsible for more than 50 confirmed fatalities between 2013 and 2015. At least six other fentanyl derivatives have been identified as well. “The danger there is the potency of that material and the ease in which people can obtain it,” says Jill M. Head, a supervisory chemist with DEA’s Special Testing & Research Laboratory.
Path to illegalization
Opioid analogs and other designer drugs present authorities with a game of Whac-A-Mole: By the time officials know enough about a molecule to start regulating it, a new generation of compounds—slightly different from those previous ones—pops up. It can be hard to keep up, Head says.
It takes an act of Congress to outlaw a drug. Though that may be the ultimate goal for the most popular and persistent synthetic drugs, there is a back door that allows authorities to bust someone for importing and distributing a designer drug that isn’t yet a controlled substance. “If it’s listed in the Controlled Substances Act, it’s illegal,” Head says. But just because a chemical isn’t listed doesn’t necessarily make it legal. The Federal Analogue Act, passed in 1986, allows any chemical that is “substantially similar” to a Schedule I or II drug—substances with a high potential for abuse—to be treated as such under the law.
Establishing similarity, Head says, requires three key components. First, it must be clear that the new drug is being manufactured for human consumption, which is typically demonstrated by showing that the chemical has no legitimate industrial or other purpose.
Next, the new drug must be structurally similar to an illegal drug. Head’s laboratory, in conjunction with DEA’s Office of Diversion Control, tackles this requirement. Her team focuses on the structural characterization of drugs seized by law enforcement agencies. Her methods include nuclear magnetic resonance spectroscopy, mass fragmentation mass spectrometry, and a time-of-flight mass spectrometry approach that leaves the chemical intact. “We use some sort of combination of those three techniques to elucidate an unknown drug structure,” she says.
The third criterion is that the new drug acts on the brain in the same way as one of the listed drugs. That’s where laboratories such as Baumann’s and other investigators’ come in.
Before Baumann began studying designer drugs, his laboratory at NIDA was involved in developing medications to treat substance abuse disorders, trying to find stimulants that lack addictive properties but curb an appetite for cocaine. As the designer drug epidemic began to unfold in 2012, Baumann saw there was a major knowledge gap: Are these drugs addictive? Are they dangerous? What is their potency? What do they do to the brain? He realized that his lab could use the same methods they’d been employing to find antiaddiction medications to study designer drugs.
So he went to his bosses to request a radical change in direction for the laboratory. “We repurposed the laboratory to start looking at all these new drugs on the street,” he says.
To determine whether a new designer drug mimics the actions of a conventional drug, Baumann’s team identifies the new drug’s molecular targets in the brain and then analyzes whether it interacts with that target in the same way as the conventional drug. For example, most addictive stimulants interact with transporter proteins that move dopamine from synapses back into neurons. Cocaine blocks the dopamine transporter, increasing dopamine levels in synapses by preventing dopamine from reentering the cells. Amphetamine also targets the dopamine transporter and increases dopamine levels, but it does that by entering neurons to facilitate dopamine release. If a new drug acts on transporters in the same way as an existing controlled substance, then there’s a good argument to be made that they are, for the purposes of the law, the same.
To spot transporter blockers and releasers, the scientists first grab some rat brain. They manually grind it up with a device that resembles a mortar and pestle and then suspend the brain matter in an aqueous solution. After the suspension is placed in a centrifuge, the separated liquid contains the goods: synaptosomes, which are isolated membrane-bound nerve endings.
To identify drugs that are cocainelike transporter blockers, the researchers add radiolabeled dopamine to synaptosomes at the same time as the designer drug; if the drug blocks transporters, the radiolabeled dopamine doesn’t get taken up into the synaptosomes and so remains outside. To identify amphetamine-like releasers, the researchers first preload the synaptosomes with radiolabeled dopamine, then add the drug. If the drug is a dopamine releaser, it reverses the normal direction of transporter flux, and the radioactive dopamine flows out of the synaptosomes. Baumann’s team measures the amount of radioactivity remaining in the synaptosomes using scintillation counting.
To complicate matters, many drugs interact with both dopamine and serotonin transporters to increase the concentrations of the neurotransmitters in the brain. “What we find is that a drug that increases dopamine a lot, that’s a bad drug. It’s going to be very addictive,” Baumann says. Drugs that selectively increase serotonin aren’t as troubling because elevated serotonin in the brain is not associated with addiction, he adds. Drugs that increase dopamine and serotonin to a similar extent produce complex behavioral effects, but generally, elevations in serotonin tend to dampen addictive effects produced by elevations in dopamine.
At this point, Baumann has studied so many synthetic drugs that he can, in some cases, predict how a particular substance will affect dopamine and serotonin levels in the brain based on the drug’s structure alone. For example, he has studied more than 100 designer stimulants called cathinones, which share a β-keto amphetamine core structure but differ with respect to three side groups. On the basis of the size and chemical structure of each of those groups, Baumann can say, before even testing the molecule, whether the new drug blocks or helps release dopamine and how well it activates the dopamine versus the serotonin transporter.
Of course, simply looking at isolated transporters or molecular structures doesn’t tell a new drug’s whole story. The missing piece is how the drug’s modulation of the relative concentrations of neurotransmitters in the brain affects behavior. For that, Baumann turns to animal studies.
Acting out
Detecting tiny fluctuations in the concentration of the neurotransmitters in rat brains is no easy task, requiring precise timing and ultrasensitive assays. Using a dialysis-like method, the scientists collect fluid samples from a rat’s brain while the animal is awake and attached to a tether. They measure concentrations of dopamine and serotonin in the fluid samples using high-pressure liquid chromatography coupled to electrochemical detection. When the scientists inject a rat with a dose of a novel drug, they can then use the ratio between increases in dopamine and serotonin to determine whether the drug behaves more like amphetamine—which only increases dopamine levels—or more like ecstasy, which ups both dopamine and serotonin levels. That’s important because an amphetamine-like drug will be more addictive, and thus a bigger problem on the street.
While the scientists collect the neurochemical data, they’re also monitoring the animal’s behavior. Peering through a windowed door as one of his chemists injects three rats with a mystery drug to initiate a dialysis experiment, Baumann studied the caged rodents’ behavior in anticipation. He says he can sometimes tell just by looking at how a rodent acts whether the drug is more like amphetamine, ecstasy, or some other narcotic. The rats started stretching out their paws and wandering around their cages, keeping low to the ground. Then, they began sniffing with side-to-side head movements. After staring intently at the rats for a minute, Baumann emphatically concludes that this is classic ecstasy-like behavior. When Baumann asked the chemist later what she’d given the rodents, his hunch was confirmed.
Baumann says they are seeing a lot of ecstasy-like designer drugs right now, but what really keeps him up at night are the synthetic opioid drugs. Flipping through his designer drug spreadsheet, Baumann pauses on the opioid section and remarks on how quickly these new substances have gone from a nonissue to a big problem. The rapid rise in synthetic opioids, which are highly addictive and carry a high risk of overdose, makes his work particularly urgent. Yet, many of these drugs are so new that there are few ways to study them, and their potency, lethality, and side effects remain unknown. But Baumann plans to change that, so that the next time a dangerous synthetic opioid gets picked up on the street and added to his spreadsheet, enforcement agents will know what they are up against.
Erika Gebel Berg is a freelance writer. A version of this story first appeared in ACS Central Science: cenm.ag/designerdrugs.





Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter