Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Cancer
Natural killer cells may mediate cancer immunotherapy
Checkpoint inhibitors may trigger more than T cells to attack cancer, researchers report in a mouse study
by Cici Zhang
September 13, 2018
| A version of this story appeared in
Volume 96, Issue 37
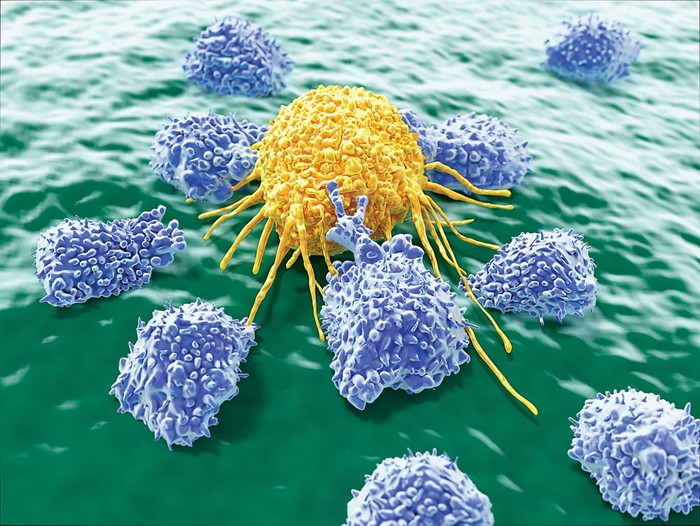
Checkpoint inhibitors have revolutionized cancer treatment by unleashing the immune system on tumor cells. These drugs’ effects have been almost exclusively attributed to responses from antitumor T cells, yet they also work in certain tumors that T cells cannot recognize, suggesting other types of cells may be at play.
A team led by cancer immunologists David H. Raulet of the University of California, Berkeley, and Michele Ardolino of the University of Ottawa and Ottawa Hospital now report that a type of lymphocyte called a natural killer (NK) cell can mediate the anticancer activity of checkpoint inhibitors in mice (J. Clin. Invest. 2018, DOI: 10.1172/jci99317).
The researchers first observed that a fraction of NK cells that had been recruited into tumors in mice expressed PD-1, the checkpoint receptor targeted by the inhibitors, suggesting that the drugs could affect the cells’ behavior. Then they gave checkpoint inhibitors to mice with NK cells but no antitumor T cells and found that the animals’ tumors still shrank. But in mice that didn’t have functional NK cells, the inhibitors’ anticancer effects were greatly reduced.
Since the findings suggest NK cells play a role in checkpoint inhibitors’ therapeutic effects, Raulet says, combining therapies that target NK cells with checkpoint blockade may be a great approach for treating various cancers, including those that T cells don’t recognize well.
Raulet is a cofounder of Dragonfly Therapeutics, which develops NK cell therapies.
Jeffrey Miller, a hematologist who studies NK cell immunotherapy at the University of Minnesota, says that although mouse and human NK cells have many differences, this study indicates researchers should explore the PD-1 pathway in human NK cells.
Jason Luke of the University of Chicago Medicine, who specializes in immunotherapy, agrees. He says that although previous clinical trials to harness NK cells have ended up with unimpressive results, the current findings suggest it may be possible to find ways to use these cells to improve patient outcomes in the future.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter