Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Neuroscience
How air pollution messes with our minds
Air pollution inflames the brain, sparking reactions that lead to diseases such as dementia and autism
by Janet Pelley, special to C&EN
May 31, 2020
| A version of this story appeared in
Volume 98, Issue 21

Neurotoxicologist Deborah Cory-Slechta had a somewhat macabre introduction to her current area of research. In 2012, a colleague at the University of Rochester kept pestering her, “You have to look at these brains!”
Günter Oberdörster studies air pollution, and he wanted Cory-Slechta to examine the brains of mice he had raised in a polluted atmosphere—specifically, a chamber filled with particles that mimic the traffic-related air pollution permeating major cities. Cory-Slechta was already known for studying the effects of neurotoxic chemicals like lead and pesticides on the brain. That’s why Oberdörster came to her. She hadn’t considered that inhaling polluted air could also cause significant brain damage, but when she looked at the brains, she was stunned. The exposed mice had brains full of inflammation and structural abnormalities. “I couldn’t find a single one that was normal,” Cory-Slechta recalls.
Air pollution exposure is well known as a driver of lung and cardiovascular diseases, including asthma and hardening of the arteries. But as dozens of epidemiological studies have suggested over the past decade, it’s also likely linked to brain conditions such as autism and dementia. Some scientists estimate that 20% of dementia cases, for example, are caused by air pollution. Now researchers like Cory-Slechta are trying to figure out why.
Researchers believe the link is inflammation, a universal problem seen in animal models exposed to air pollution and in the brains of people with autism, dementia, and other neurological conditions. Scientists are now beginning to analyze the cascade of biochemical steps triggered by inflammation in the brain to understand the mechanisms that lead to cognitive impairment and disease.
Brain on fire
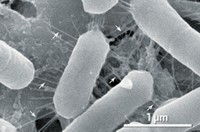
Emissions from vehicles, power plants, and factories create a complex soup of gases, organic contaminants, metals, particles, and more. The epidemiological evidence, however, points to one category of air pollution as the culprit in neurological diseases. Fine airborne particles called particulate matter (PM) from sources including vehicle traffic and wildfires are particularly problematic because they penetrate deep into the lungs, says Lucio Costa, a neurotoxicologist at the University of Washington. This fine particulate matter, which can be made up of a number of different chemicals, measures less than 2.5 µm across, earning it the scientific notation PM2.5.
Inflammation is the body’s healthy response to an injury like a sprained ankle or an infection. Sensing damage, immune cells charge in and devour dying tissue and pathogens, releasing signaling proteins called cytokines that call in more immune defenses. This is how the immune system reacts to the many substances in dirty air, too, going on the attack as if the particles were invaders. But when chronically stimulated—as happens when every breath of air, day after day, is dirty—the immune system starts damaging healthy tissue too. Air pollution exposure initiates system-wide inflammation, generates oxidative stress, and weakens the protective barrier formed by the epithelial cells that line our blood vessels. With over 90% of the world’s population chronically exposed to fine particulate air pollution at levels above the World Health Organization’s guideline of 10 μg/m3, the exposure and subsequent inflammation are a real concern.
It may seem intuitive that exposure to these irritating particles would cause lung problems—after all, that’s the first tissue in the body they penetrate. How they affect the brain is much less obvious. Scientists say these particles likely influence the brain through direct and indirect pathways. Scientists propose two main routes that directly impact the brain. In the first, particulate matter travels up the nose into the olfactory nerves that lead to the brain, where it can directly irritate the delicate tissue there. In the second, particulate matter hops into the bloodstream through the lungs and makes its way to the brain and elsewhere in the body.
Other scientists suggest that pollutants indirectly influence the brain by setting off an inflammatory cascade in lung tissue, which in turn dumps irritating substances into the bloodstream. When those get to the brain, they spark more inflammation. Following both direct and indirect pathways, scientists are starting to tease apart the molecular mechanisms by which air pollution exposure clogs our brains with plaques, kills neurons, and warps the architecture of developing tissue.
One of those scientists, Cory-Slechta, noticed some commonalities between mice and people. As she and Oberdörster continued their collaboration, they reported that infant mice exposed to air pollution had altered social behaviors similar to those of children with autism. In death, the mice had brains that showed signs of inflammation and reduced amounts of white matter, which conducts messages from one neuron to another and between distant parts of the brain. The mice also had enlarged brain ventricles—cavities containing cerebrospinal fluid. And male mice were more often affected than females. All these behavioral and physical characteristics mirrored those of children with autism and attention deficit disorder. For instance, autism more often affects males than females.
Cory-Slechta checked the air filters on the chambers where the mice had been exposed to air pollution. What she found was that they were loaded with iron, a frequent trace contaminant in air arising from combustion sources and vehicle friction. Her team had piped particulate matter they’d collected from the air outside their urban laboratory building into the mouse growth chambers.
Knowing that in excess amounts, ferrous iron (Fe2+) induces inflammation and oxidative stress in cells and kills them, Cory-Slechta wondered if the iron-laden air was driving the loss of white matter in the animals’ brains. Her lab had shown in the past that ultrafine air pollution particles—those less than 0.1 μm in diameter—can introduce iron to brain cells.
A follow-up experiment by her team linked trace amounts of iron in particulate air pollution to elevated levels of iron in the olfactory nerves and brains of mice (Toxicol. Pathol. 2019, DOI: 10.1177/0192623319878400). Taken together, all the results hint that the mice might be suffering from brain cell death driven by iron toxicity, Cory-Slechta says. While iron-driven cell death in humans has been found in neurodegenerative diseases such as Parkinson’s and Alzheimer’s, its role in neurodevelopmental disorders like autism has not been investigated.
Cory-Slechta says that if future experiments confirm her findings, they raise questions about regulatory policies. Currently, the only metal for which the US Environmental Protection Agency has set air quality standards is lead, but there are other neurotoxic metals in air pollution that could be considered for regulation, she says. The European Union has set air quality standards for cadmium, lead, arsenic, and nickel, all of which are neurotoxic.
Many cities across the world have levels of air pollution above the guideline set by the World Health Organization.
Source: IQAir. Note: PM2.5 is particulate matter with a diameter less than 2.5 μm. It can negatively affect health when breathed in

Altered proteins
Other researchers are investigating the molecular mechanisms that tie particulate matter exposure to dementia. Neurological diseases like Alzheimer’s that have dementia as a symptom are associated with sticky protein fragments in the brain called amyloid-β that cluster into plaques. One hypothesis is that the plaques disrupt communication between brain cells and eventually kill them.
Amyloid plaques contain many of the same inflammatory proteins found in fatty plaques that grow on the diseased arteries of people with cardiovascular disorders. Pondering the fact that arterial plaques are associated with air pollution exposure, University of Southern California neurobiologist Caleb Finch wondered if the same were true in the brain.
Finch and his team knew that amyloid-β is generated when enzymes snip apart amyloid precursor proteins that reside on lipid rafts in brain cells. Earlier research had shown that oxidative damage of lipid rafts increases levels of amyloid-β.
Could inflammatory processes driven by air pollution be boosting the production of amyloid-β plaques associated with dementia? Finch decided to test this hypothesis on mice genetically engineered to develop plaques in their brains.

Finch and his team raised mice in chambers containing diesel exhaust at particle concentrations seen on a daily basis in heavily polluted cities such as New Delhi and Beijing. Their brains contained 45% more amyloid-β plaques than mice raised in clean, filtered air. The researchers did not test the mice for cognition. The scientists linked this increased plaque level to an inflammatory process. The oxidative stress from the diesel exhaust, a sign of immune overreaction, altered the rafts of lipids in mouse brain cells to make more amyloid-β protein fragments.
Finch suspects that the inflammatory oxidation he observed originated indirectly via irritation of the lung surface by air pollution, but his work doesn’t directly make that tie. He points to other researchers who are providing evidence for such a link, however.
Matthew Campen, a toxicologist at the University of New Mexico, is investigating the inflammatory link between the lung and brain. He’s particularly focused on a group of enzymes called metalloproteinases made by immune cells. These enzymes play an important role in normal tissue growth and death, but when the immune system is overstimulated, they can cause unwanted tissue destruction. “The metalloproteinases chew up the normal proteins that coat and support lung cells, generating protein fragments that we look at as ‘molecular shrapnel,’ ” Campen says. When the fragments from these proteins enter the bloodstream, the endothelial cells lining the blood vessels see them as an indicator of damage somewhere in the body and respond with inflammation, which makes the cells leaky.
Campen and his team had shown in earlier work that cleaved lung proteins penetrate the blood-brain barrier and activate the brain’s immune cells (Proc. Natl. Acad. Sci. U.S.A. 2017, DOI: 10.1073/pnas.1616070114). “These molecules impair the functioning of neurons, so the brain’s immune cells come over and try to shore up defenses,” Campen says. Normally, the brain’s immune cells clean up contaminants and plaque proteins, improving communication between neurons. But if they are chronically stimulated, they generate neuroinflammation and oxidative stress while ignoring their usual clean-up roles.
Exposing mice to ultrafine particulate matter, Campen’s lab recently identified some of the hundreds of different kinds of protein fragments generated by irritated lungs. These proteins yield fragments that remain biologically active, binding to endothelial cells and switching on production of proteins associated with inflammatory diseases (Part. Fibre Toxicol. 2019, DOI: 10.1186/s12989-019-0304-6). Campen and his team want to identify more of those proteins, then see if they can scavenge the fragments from the blood, a move that could one day lead to therapies to reduce systemic inflammation.
Other researchers are exploring the effect of particulate matter exposure on the developing brain during pregnancy—particularly in autism. People with autism spectrum disorder typically have reduced social and communication skills, along with difficulty in learning. Affected children have unusual brain structure and higher levels of inflammation and oxidative stress compared with their peers.
Epidemiology studies have shown a strong link between autism spectrum disorder in children and their mothers’ exposure to air pollution during pregnancy. The University of Washington’s Costa has seen this association in animal experiments too. His team has shown that mice exposed to diesel exhaust display unusual social interactions, altered brain structure, and oxidative stress. These mice also have lower concentrations of the brain protein reelin than mice not exposed to diesel exhaust.
Scientists suspect reelin plays an important role in autism. Reelin helps organize the structure of the brain, directing the proper layering of neurons. After exposing developing mice to diesel exhaust, the scientists detected high levels of inflammatory proteins called cytokines, which block reelin production. Exposed mice not only made less reelin, they made it in areas of the brain outside of the normal distribution, hinting that neurons had not been guided to their final, appropriate destination during brain development (Brain, Behav., Immun. 2019, DOI: 10.1016/j.bbi.2019.01.013).
Costa emphasizes that his research is just one example of the myriad consequences of neuroinflammation and oxidative stress and that there are many more waiting to be discovered. He believes that more work needs to be done on the interactions between genes and the environment to explain why some people are vulnerable to traffic exhaust while others aren’t.
Advertisement
“Mechanistic studies are increasing our understanding of air pollution and its effects on the brain and may also lead to therapies,” Costa says. But the research must go hand-in-hand with measures to reduce air pollution, he adds. This fact is especially true for developing countries such as China and India. But even in the US, where air is relatively clean, monitoring reveals that in 2019 more than 53.3 million people suffered unhealthy spikes of fine particles, mainly due to wildfires. And a growing body of research suggests that there is no safe level of PM2.5. At the same time, the US government in April announced that it would not tighten controls on PM2.5, retaining the 2012 standard to protect public health at 12 µg/m3 despite the finding by EPA scientists that a standard of 9 µg/m3 would cut annual deaths from air pollution by about 27%.
The cognitive impacts of air pollution rarely, if ever, get mentioned in policy debates. Scientists would like to see that change. Researchers say they are building evidence that air pollution is a serious threat to the brain health of the most vulnerable—babies, children, and the elderly.
Meanwhile, Cory-Slechta has a freezer full of mouse brains waiting to be analyzed, potentially yielding data that can be used to strengthen this argument and, she hopes, help protect our brains.
Janet Pelley is a freelance science writer based in Canada.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter