Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Climate Change
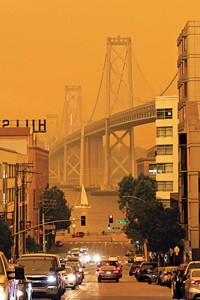
Wildfire smoke may cause more asthma hospitalizations than other forms of particulate pollution
As wildfire season grows longer, scientists want to understand the health effects of the resulting smoke
by Katherine Bourzac
April 11, 2019
| A version of this story appeared in
Volume 97, Issue 15

Wildfire seasons in the US continue to get longer, and the fires themselves are getting larger and more intense, in large part because of climate change. This trend will continue to fill the air with smoke, particularly in the western US. Epidemiologists are rushing to understand the possible public health impacts of breathing in this smoke.
One major open question is whether the fine particulate matter carried in wildfire smoke affects health differently than the particles released from other sources, such as vehicle tailpipes. The first large-scale study of the issue suggests that different health effects may occur, finding that wildfire smoke caused more hospitalizations due to asthma, wheezing, and bronchitis than other sources of particulate pollution (Environ. Health Perspect. 2019, DOI: 10.1289/EHP3860).
Exposure to particulate matter smaller than 2.5 µm in diameter (PM2.5) can cause cardiovascular and respiratory problems, according to the US Environmental Protection Agency. The effects of PM2.5 pollution on health have been studied mostly in an urban context, where it’s emitted by industrial facilities and vehicles.
PM2.5 in wildfire smoke likely has a different chemical composition than the particles released in urban pollution. Also, in wildfires, particles are emitted at higher concentrations over shorter periods of time, says Ana Rappold, an epidemiologist at the EPA’s National Health and Environmental Effects Research Laboratory.
Most studies on the health effects of wildfire PM2.5 have examined single fires. So Rappold and her colleagues did a more sweeping study, examining hospitalizations of Medicare patients 65 years or older on days with high PM2.5 exposure levels, due to both wildfire smoke and other sources, from 2008 through 2010 across the US.
They compared high-PM2.5 days with days when the air was clear. On smoky high-PM2.5days, there were 6.9% more hospitalizations due to asthma, wheezing, and bronchitis than on clear days, whereas non-smoky high PM2.5 days had only 1.3% more asthma admissions on nonsmoky days with comparable PM2.5 exposure levels.
These studies are challenging because researchers haven’t settled on a universal metric for smoke exposure. Researchers are still figuring out how to define smoky days in health studies, says University of Montana epidemiologist Curtis Noonan.
Speaking at a workshop held by the Institute for Journalism & Natural Resources in Missoula, Montana, on April 5, University of Montana computational ecologist Erin Landguth noted that the lack of air-quality monitoring stations in rural areas is another challenge for these studies. Her group has found a possible link between wildfire smoke exposure and influenza rates in 51 of the state’s 56 counties. She is planning more detailed studies that will take advantage of local electronic medical records and a denser sensor network being installed in the Missoula Valley.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter