Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biomaterials
Low-cost biodegradable foam could heal chronic wounds
In animal tests, the synthetic material works as well as the best wound-care technology
by Prachi Patel, special to C&EN
April 27, 2022
| A version of this story appeared in
Volume 100, Issue 15

A new synthetic foam works just as well as the leading gold-standard biological materials in closing up chronic wounds in animal tests, but should cost 75% less (Sci. Transl. Med. 2022, DOI: 10.1126/scitranslmed.abm6586). The biodegradable material soothes inflammation and is also an antioxidant. It could bring down the cost of treating chronic wounds, which affect around 4.5 million people in the United States alone.
Diabetes, obesity and vascular disease all predispose people to wounds that don’t heal on their own, says Craig Duvall, a bioengineer at Vanderbilt University who led the new work. Chronic wounds, he says, “can be painful, susceptible to infection, and can lead to amputations.”
Doctors treat these wounds with scaffolds that cover and protect the site from infection while allowing cells to infiltrate and grow new tissue. Wound-healing products available today are typically made of expensive biological materials such as collagen, which comes from animals, or hyaluronic acid, which is made by fermentation. Less expensive, mass-manufactured polyester scaffolds break down in the body to form acidic byproducts that can trigger inflammation. “They don’t really synergize with the body,” says Duvall.
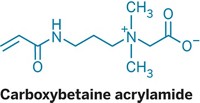
So he and his colleagues made highly porous foams from a more biocompatible synthetic polymer, polythioketal urethane (PTK-UR), which Duvall’s group invented eight years ago for making tissue engineering scaffolds (Biomaterials 2014, DOI: 10.1016/j.biomaterials.2014.01.026). These foams are broken down by reactive oxygen species (ROS) into small hydrophilic ethylene glycol fragments that are readily resorbed from the wound bed. Chronic wounds are known to have excessive ROS that damage cells and inhibit healing. The PTK-UR foam, Duvall thought, would act as an antioxidant to soak up the ROS produced by infiltrating cells, which would both detoxify the wound environment and naturally break down the foam as new tissue forms.
The researchers made four foams with different hydrophilicities by tweaking the polymer chemistries. In saline tests, the more hydrophilic foams removed more ROS and degraded faster than less hydrophilic films because they soaked up more fluid.
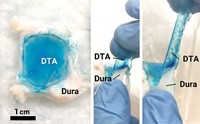
Next, the researchers tested the foams in skin wounds on a pig, which closely resemble human skin wounds. The most hydrophilic material showed 70% wound closure after 24 days. They compared this foam with a commercial collagen-based scaffold that costs $3,855 for a 129 cm2 patch, and a commercial synthetic foam costing about $850 for a 100 cm2 patch. The new material’s performance was comparable to that of the collagen scaffold in further tests on porcine skin wounds, but Duvall says its cost should be comparable to that of the commercial synthetic foam.
“Our material seems to beat current standard products that are synthetic and behaves at least as well as current biological products,” he says.
The results provide “compelling evidence that the synthetic polythioketal urethane foam possesses impressive ability to improve the healing process,” says Chandan K. Sen, a physiologist and executive director of the Comprehensive Wound Center at the Indiana University School of Medicine. The foam will need to be tested further to assess its effectiveness on complicated infected wounds, he says. However, based on the evidence so far, he hopes it will translate to a better wound care option.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter