Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Drug Delivery
These scientists want to engineer breast-milk cells to deliver drugs to babies. Here's how.
Katie Whitehead and her team at Carnegie Mellon University will start with goat-milk cells to see if they can carry therapeutic payloads
by Megha Satyanarayana
February 27, 2019
| A version of this story appeared in
Volume 97, Issue 9

Elsie is a consistent producer. Ebony is pretty hit or miss. But Charlotte—black and tan, with the perkiest ears—she’s prolific. She’s one reason why, every few weeks, a graduate student named Rose Doerfler wakes up at the crack of dawn to drive the winding roads outside Pittsburgh to Goat Rodeo Farm and Dairy.
On this December morning, Doerfler will gather milk from the capricious capridsof this cheese-making farm, rush back to Katie Whitehead’s lab at Carnegie Mellon University, and carefully isolate the cells that float in the white, fatty murk.
“I’m optimistic,” Doerfler says. “Charlotte did pretty well for me last time.”
What Doerfler does with this milk is the first step in Whitehead’s grand plan to one day turn human breast milk into a drug-delivery device for sick babies. The goat milk will serve as a model for human milk, with mice as a model for babies. She’ll track goat-milk cells as they enter a mouse and do experiments to see if the cells can carry therapeutic payloads.
If this sounds kind of out there, Whitehead wants it that way. After the sting of having a grant rejected in 2016 because her ideas were “not innovative,” she decided to prove the reviewer wrong. While nursing her infant daughter, she thought about what breast milk was and what it was giving her child. From there, the idea came into focus in bits and pieces.
Cell engineering is changing the way we treat disease, she thought. Look at cancer treatments that involve modified T cells. Human breast milk is full of cells. Surely, she thought, we can isolate them, engineer them to become potent vehicles for medicine delivery, and feed them to babies quickly and efficiently. Less poking and prodding, she thought, and less pain.
Coupling modern medicine to this most intimate and iconic act of motherhood could lead to a new wave of therapies and oral vaccines, she says in her grant proposal. Whitehead believes that she can engineer immune cells in breast milk so that they can deliver vaccines, or engineer stem cells in breast milk to fix certain birth defects. She could also engineer epithelial cells in breast milk to coax them into producing proteins that some babies cannot make, offering what could be a lifelong fix for some serious genetic diseases. For instance, in phenylketonuria, babies lack an enzyme that breaks down phenylalanine. The project could also help answer a slew of questions about the biology of breast milk and infant feeding.
The idea was a winner. In 2018, Whitehead, a chemical engineer who studies drug delivery, earned a National Institutes of Health Director’s New Innovator Awardto apply cell-engineering principles to breast milk. Finally, she was being recognized for big, bold thinking. And yet she wondered: Breast feeding is one of the oldest acts of humanity. Why are these questions bold? By 2018, shouldn’t we already know what breast milk is capable of doing?
“The basic biology isn’t revolutionary. It’s there, waiting to be discovered,” Whitehead says.
She wondered whether it hasn’t yet been explored because, historically, women haven’t been in leadership positions, applying, as scientists often do, their life experiences to their work. “I think it’s because the women aren’t doing the science. I really think that’s the unfortunate answer.”
Whether this project succeeds or fails, Whitehead says she hopes to get across that this is the tip of the iceberg when it comes to unanswered questions about female biology. She also hopes to encourage more women to let personal experiences shape our pursuit of science. This diversity in thinking will lead to broader questions, more discovery, and, of course, more innovation.
“I’m in my sixth year now of being a professor, and in the beginning I kind of thought, ‘OK, I have to work on certain types of problems and certain types of diseases.’ I have found it to be only somewhat fulfilling,” she says as she waits to hear from Doerfler about the goat-milk cells she isolated that morning. “So to feel like there’s this additional level of meaning that I can bring to my work—it’s been really priceless.”

First, follow the cells
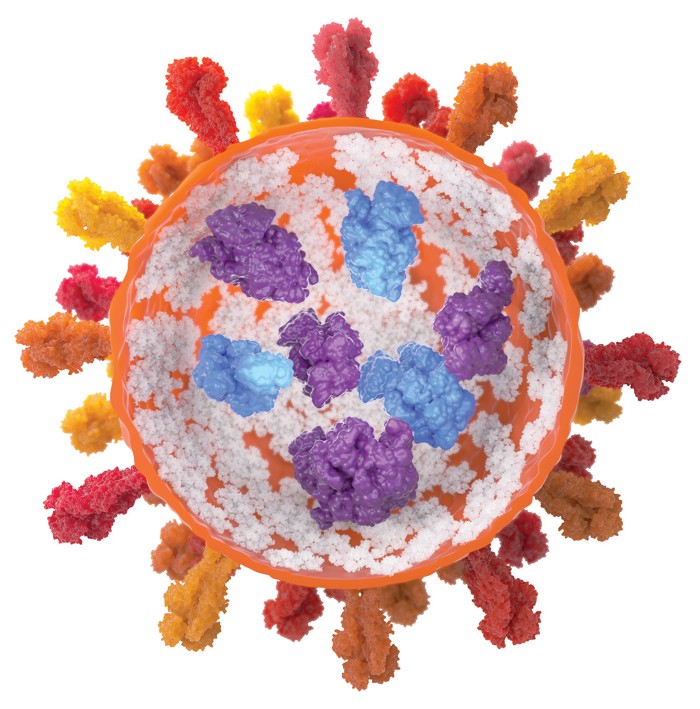
Breast milk is a combination of carbohydrates, fats, proteins, nucleic acids, microbes, and a surprising number of cells from the woman who produced it. Carlito Lebrilla, an analytical chemist at the University of California, Davis, calls it “nature’s delivery device.” He’s been parsing the oligosaccharide components of breast milk for years and learning how pervasive milk compounds are in a baby’s body. “We’ve looked at the blood of infants, the urine of infants, the saliva, the stool—and the components of milk are everywhere,” he says.
Lebrilla’s efforts to track the molecular components of breast milk are akin to what Whitehead is trying to do with cells. She wants to know: Where do the cells from breast milk go in a baby’s body? Babies’ stomachs are less acidic than adults’, and their immature digestive tracts are leaky enough for cells to slip through.
Armed with information about where breast-milk cells go in an infant’s body, Whitehead says, she may be able to devise organ-specific treatments. She envisions taking breast milk from a mother with a sick child, isolating the cells, transfecting them with DNA corresponding to therapeutic proteins or vaccines, allowing the cells to grow and divide, then putting them back in the milk, and feeding that medically fortified milk to the child. Evidence with other cell types in breast milk suggests that it’s possible that these treatments could be lifelong—breast-milk cells can integrate into the organs of the child drinking them.
“My vision for them has been that they will essentially be protein-replacement factories. Epithelial cells are literally protein-production factories, so why not use them as such?” she says.
Of the three main types of cells found in human breast milk—epithelial, immune, and stem—Whitehead and her team are starting their experiments with epithelial cells, which line our organs and blood vessels. As the most abundant, they seemed like a good first choice to engineer.
This is where Charlotte, Elsie, and some of their sisters come in. One of Doerfler’s first tasks in Whitehead’s lab was to find a substantial source of breast-milk cells to study. Working with human breast milk would require complex protocols and ethics approvals, and it would be hard to develop a standard set of cells because humans vary in their diet and medication use. So Doerfler needed to look elsewhere.
Although mice make good test subjects for her work, including testing engineered cells in later experimental stages, “you can’t get very much milk from mice,” Doerfler deadpans.
After calling several farms just outside Pittsburgh, she learned about Goat Rodeo. Owner India Loevner was intrigued.
“People don’t realize how closely related mammals who make milk are,” Loevner says.
Loevner agreed to participate, and Doerfler began her periodic trek to the farm to collect samples during the morning milking session. She soon learned that a goat whose milk makes delicious cheese isn’t always going to be the same goat that produces a lot of cells in its milk.
Back in the lab after that morning trip in December, Doerfler spun Charlotte’s milk in a centrifuge and skimmed off the fat. At the bottom of the centrifuge tube was a thick layer of cells. She was pleased. As winter settled on southwest Pennsylvania, she got to work counting the cells so she could plan an experiment to put fluorescently tagged nanoparticles in them that would eventually help the lab track where the cells go.
“These look nice,” she says, pointing to plump little blobs under a microscope on a counting grid.
Tracking breast-milk cells after they’ve been fed to an animal is not without precedent. Immune cells from breast milk have been found in the liver and spleen, among other places. And several years ago, Foteini Hassiotou Kakulas, a cell biologist at the University of Western Australia, tracked the movements of stem cells from human breast milk in the body of a mouse.
Where the cells journeyed in the body was surprising. “We are not just talking about easy-to-access organs, but also isolated and well-protected organs such as the brain,” Kakulas says. “They integrate and become part of the normal function of these organs. It’s an amazing phenomenon.”
Kakulas also discovered that breast-milk cells, predominantly the epithelial ones, produce large amounts of a specific type of RNA that prevents messenger RNA from being translated into a protein. These RNAs largely control maternal genes. But Kakulas thinks that they, like most other elements of breast milk, have a mission inside a baby—influencing newborn and infant development by tamping down protein production related to, for example, thirst or hunger (Int. J. Mol. Sci. 2016,DOI: 10.3390/ijms17060956).
Advertisement
Kakulas sees a lot of potential in Whitehead’s idea, but also a lot of risk.
“Breast-milk-cell research using modern techniques is relatively new and has a lot of promise in the medical field,” she says. But “a lot of work will be required to ensure the safety of such a system in babies. Preterm babies and babies at risk are likely wonderful candidates in a research area such as this.”
Lebrilla agrees that the idea is exciting.
“Milk is just an incredible resource for interesting particles and delivery devices, and I think people should really look at it more closely.”

Second, get more women in science
For Whitehead, one of the side effects of the work she’s put into the New Innovator Award has been a reckoning about the direction of her lab’s focus. Before breast milk, her lab worked on drug delivery in a more general way, focusing on designing proteins for oral delivery or finding ways to transport RNA therapeutics. That work, she says, was less viscerally related to personal experience.
But with the breast-milk proposal, as well as another in the lab exploring how to package drugs in such a way that they can’t cross the placenta, there has been a subtle shift toward addressing major problems that affect women’s health during their reproductive years.
The experience of pregnancy, childbirth, and breastfeeding has laid bare for Whitehead the difficulties of doing research on pregnant women, fetuses, and children. Take the placenta project: most drugs have not and—with currently available technology—cannot easily be tested for fetal safety. Many pregnant women must make choices about taking medicines they might need without knowing if those medications are safe for their babies.
“Yes, it is absolutely true that there are very limited means by which to conduct ethical trials of any kind on this,” she says of drug safety during pregnancy. But the people with the most institutional power are men, who underestimate the problem because they haven’t experienced it themselves, she contends.
“I think the other large part of the problem is that there are a bunch of male scientists sitting around saying, ‘Nobody’s dying here,’ ” she says, so the quality-of-life issue gets lost.
Lebrilla says a broader cultural shift needs to happen in biomedical science for research on underserved topics like breast milk to become more pervasive.
“Certainly, I think having more women in science will change it in a big way,” he says. But the problem is a bigger one of where we place our value. Biomedical science is focused on cures, he says, and less on prevention. And the messengers of prevention, the primary care doctors, the nurses, the dietitians, tend to be women. The work of prevention ends up being devalued, he says. And while Whitehead wants to cure disease, she wants to do it at the earliest point possible, through breast milk, or maybe formula, which the child would be getting anyway. In doing this, she hopes to prevent illnesses that often lead to disability or death, or prevent children and their families from having to go through years of painful and potentially costly treatments.
And so Charlotte, Elsie, Ebony, and the sisterhood of Goat Rodeo Farm find themselves part of not just a scientific project but a social one as well. Whitehead hopes that understanding more about breast milk and other aspects of women’s biology will normalize women’s biology as a space where chemical engineering can solve problems, but she doesn’t believe that failure will kill that vibe.
“I believe the breast-milk proposal will serve 100% of the population,” she says. “Everyone is born. Everyone has the potential to use this type of therapy. Our main goal is to create new technology that works. And so, even if I fail, if I can inspire others to go forth and to start asking questions along these lines, then it’s a win, regardless of what happens to me.”



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter