Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Neuroscience
FDA green-lights lecanemab to treat Alzheimer’s disease
The developers list an annual price of $26,500 per patient
by Shi En Kim
January 10, 2023

In a decision that surprised no one, the US Food and Drug Administration granted accelerated approval to the Alzheimer’s drug lecanemab, marketed as Leqembi. Last year, its developers Biogen and Eisai notched positive Phase 3 results that surpassed all other monoclonal antibody drug candidates. Lecanemab slowed cognitive decline among trial participants by 27% relative to the placebo.
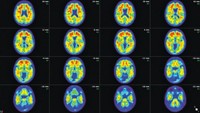
According to the FDA statement on its decision, a lecanemab prescription must come with a warning of the possible side effects of amyloid-related imaging abnormalities (ARIA), which are swelling and bleeding in the brain that can be detected by magnetic resonance imaging. During Phase 3 clinical trials, ARIA occurred in about 21% of participants, Eisai reported.
Biogen and Eisai announced an annual price tag for lecanemab of $26,500. The companies’ previous Alzheimer’s drug, aducanumab or Aduhelm, gained US Food and Drug Administration approval and debuted on the market at a per-patient annual cost of $56,000 despite inconsistent results during clinical trials. Swift public backlash prompted the developers to halve the price. But in early 2022, US Centers for Medicare and Medicaid Services (CMS) declined to cover Alzheimer’s monoclonal antibody treatments, including aducanumab, except in clinical trial settings, thereby limiting treatment access among the patient population. As it stands, this decision applies to lecanemab.
An independent report by the Institute for Clinical and Economic Review (ICER) estimated that a reasonable price for lecanemab would be between $8,500 and $20,600 per patient per year. But even the upper threshold is already an overvaluation, says David Rind, ICER’s chief medical officer who was on the team that crunched the numbers. “The current price of $26,500 would not meet typical thresholds of cost-effectiveness,” he says via email.
Eisai says their pricing is justified. “Our pricing approach takes into account not only the societal value of Leqembi, but also patient affordability and health system sustainability,” an Eisai representative said in the media briefing. “When it comes to the very high unmet need and the gravity of the disease, there has been recommendations for the use of a higher willingness-to-pay threshold. And definitely this is the case for Alzheimer’s disease.”
Even a cost on the lower end of ICER’s range could translate to a huge overall spending by society on just one drug, given that over 6 million people in America have Alzheimer’s disease, Rind says in an interview. Moreover, lecanemab only delays disease progression and isn’t a cure. “I’d rather have [lecanemab] than not, but I’m not viewing that as life changing,” he says. “A drug that reversed Alzheimer’s would be worth a lot more.”
However, even with limited treatment options on the market, people with Alzheimer’s won’t immediately be stampeding towards lecanemab, says Anton Pjetur Porsteinsson, a clinical researcher at the University of Rochester Medical Center who has been involved in clinical trials of multiple monoclonal antibody candidates to treat Alzheimer’s. According to its label, lecanemab is intended only for early-stage Alzheimer’s patients with mild disease symptoms, so not every patient is eligible. Patients best poised to reap lecanemab’s benefits are those that match the profiles of participants in the drug’s Phase 3 clinical trials: Alzheimer’s patients with amyloid indications, lacking certain genetic risk factors, and not taking anticoagulants. Investigators suspect that anticoagulants contributed to at least 2 deaths during clinical trials, according to the media reports. Some patients might decline lecanemab for fear of the ARIA risks, Porsteinsson says. He estimates that about 10% of people who qualify for lecenamab will sign up in the first year. Eisai predicts that 100,000 individuals will take the drug by 2026.
Three days after the FDA announcement, Eisai filed for full approval for lecanemab. The company also said that it is working with CMS to open up access for Medicare beneficiaries, a step towards reversing the agency’s blanket decision on monoclonal antibody coverage after the aducanumab controversy. For CMS to refuse lecanemab coverage “would be a grave error,” Porsteinsson says.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter