Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Oncology
The curious DNA circles that make treating cancer so hard
Scientists are examining long-ignored extrachromosomal DNA to understand how cancer evolves resistance to drugs. Can the clues help us outfox cancer itself?
by Ryan Cross
October 18, 2020
| A version of this story appeared in
Volume 98, Issue 40

To the untrained eye, the tiny spots in the tumor cell wouldn’t look like much. In fact, other scientists had noticed them in cancer before but had generally dismissed them as a mere curiosity. But to Paul Mischel, the fuzzy dots he saw under the microscope offered a tantalizing explanation for why some cancers are so hard to treat.
In brief
In 1965, scientists saw little pieces of DNA floating around chromosomes in cancer cells. They didn’t know what to make of them, and for decades they were largely ignored. But work in the past 10 years suggests those DNA tidbits, which are circular, aren’t just some cellular debris. Cancer cells use the circles to rapidly grab or shed genes linked to tumor growth and drug resistance. These circles, now known as extrachromosomal DNA (ecDNA), may explain why some tumors, like glioblastoma, are notoriously difficult to treat, and there’s already one biotech company that thinks ecDNA will be the next big thing in cancer drug discovery.
Mischel first noticed the spots almost a decade ago while studying tumors that had gene amplifications, a mutation characterized by multiple copies of a gene linked to cancer growth. Those extra copies cause cells to churn out proteins that encourage the tumor to keep expanding. Scientists had assumed the copies were stacked back to back amid the other genes on our X-shaped chromosomes, as if the same page had been accidentally printed over and over in the middle of a book. Mischel stained the gene amplifications red and the cancer cell’s chromosomes blue. If conventional wisdom held, his microscope would reveal a glob of red dotting one of the blue chromosomes. Instead, the physician-scientist saw dozens of small red dots scattered outside the chromosomes. It was as if someone had photocopied a page from the book and then tossed the copies in the air.
Human cells are not supposed to have extra bits of DNA floating around, so Mischel described the peculiar substance as extrachromosomal DNA, or ecDNA. He had a hunch that this was not simply some genetic debris and spent the better part of the next decade trying to figure out what that ecDNA was doing in cancer.
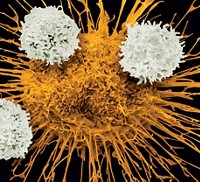
The answer turned out to be even weirder than he’d first imagined. Mischel, who is now at the Ludwig Institute for Cancer Research and the University of California San Diego, has since demonstrated that ecDNA carries cancer-promoting genes and that its circular shape fuels aggressive growth streaks and drug resistance. Just last year, he published a photo that clearly shows these circles next to X-shaped chromosomes in a cancer cell.
Today, Mischel is at the center of a small field devoted to studying the circles; it is populated by scientists who, like Mischel, stumbled upon the oddity in the course of their own research. Now that cancer researchers are looking for DNA circles, they see them everywhere. “These things have been hiding in plain sight,” Mischel says. In a study published in August of 3,200 people, he and his colleagues provide evidence that ecDNA exists in at least 15% of tumors and is much more common in certain cancers—like breast, cervical, and esophageal cancers and a lethal kind of brain tumor called glioblastoma.
More importantly, people with ecDNA in their tumors have some of the lowest 5-year survival rates, Mischel says. “These are the patients who are not responding well to the current armamentarium of even the most innovative therapies.”
He and others have set out to answer the many fundamental questions about ecDNA: Where does it come from? How does it spur drug resistance in tumors? What new tools do we need to study it? And, most pressingly for people with cancer, can a drug get rid of it?
DNA circles have changed the way Mischel thinks about cancer, and he hopes that they will soon change the way doctors think about treating cancer too. In 2018, he helped form a company, Boundless Bio, to develop drugs that target ecDNA-dependent tumors. Biotech-investor interest in the budding field suggests that other start-ups are sure to follow.
“The importance of the field is going to be predicated on how it leads to new insights for therapies,” says David Pellman, a pediatric oncologist and cell biologist at the Dana-Farber Cancer Institute. Right now, ecDNA is just an elegant explanation for how some tumors so deftly resist treatment. “So it is important to know about it, but it would be even more important if we could do something about it.”
ecDNA comes full circle
In 1965, British oncologists discovered tiny dots of DNA surrounding the chromosomes of tumor cells. They gave the strange structures a stranger name: double minutes—double because the dots were found in pairs, and minute because they were minuscule. Today, scientists think that double minutes are likely just DNA circles caught in the act of replicating.
In the 1980s and 1990s, scientists found that some of these structures contained gene amplifications and that the circles were linked to drug resistance in tumors. In 1997, Geoffrey Wahl, a cancer biologist at the Salk Institute for Biological Studies, cofounded a company called NewBiotics to look for drugs that could eliminate double minutes from cells. The idea never took off. “The Human Genome Project in the nineties sucked a lot of the oxygen out of the room,” Wahl says.

The advent of gene sequencing meant scientists were less concerned with odd observations under the microscope than with their newfound ability to scan for mutations in cancer’s genetic code. Yet sometimes that code raised questions that scientists couldn’t answer. Like why a class of drugs called EGFR inhibitors didn’t always shrink tumors in people with mutations in a gene called EGFR. Biologists knew that EGFR mutations spurred aggressive tumor growth, especially when the gene was amplified. EGFR amplifications are common in glioblastoma, but the inhibitors often do little to help people with these brain tumors. “And that was bedeviling,” Mischel says.
Mischel set out to explain this paradox and in 2010 noticed something strange: the tumors were a mixture of cells, some with lots of the EGFR gene and others with very little. So he decided to take these two types of cells and grow them in their own petri dishes to see what would happen.
It almost seemed like a silly experiment.
“Everything that we know about classical genetics says that mother cells should give rise to daughter cells that are genetically like them,” Mischel explains. Instead, the two different mother cells created tumors that looked the same: both had some cells with tons of EGFR, some with little, and some in between. “And that didn’t make any sense by classical genetics.”
So Mischel returned to old-fashioned microscopy to see what was going on in those cells. When our cells get ready to divide, our genome is neatly packed into our 23 pairs of chromosomes, which line up before being carefully allocated into two daughter cells. This moment gives scientists a chance to inspect chromosomes under a microscope and see if something is amiss. By staining the EGFR gene red and the chromosomes blue, Mischel discovered that the cells were littered with what he decided to call ecDNA—the red dots. When the cells were treated with an EGFR inhibitor, the red dots disappeared. When the drug was removed, the red dots came roaring back.
The study was published in Science in 2013 to “a colossal scratching of heads,” Mischel says. “People didn’t quite know what to make of it.”
Mischel soon homed in on a unique feature that helped explain ecDNA’s weirdness. The circles lacked centromeres, handholds that are normally found at the center of every chromosome and are essential for evenly dividing DNA between daughter cells. Without centromeres, a cell has no way to nicely divvy up circular DNA between its progeny, and the circles are dispersed at random. One cell can easily end up with more circles than the other, and as the tumor grows, it becomes a patchwork of cells—some with lots of ecDNA, some with very little, and some in between.
This unequal distribution also helped Mischel understand how the glioblastoma tumors that are treated with EGFR inhibitors bounced back so quickly. Cells with lots of the DNA circles were hit hard by the drug; apparently, they had become dependent on their EGFR amplifications. The cells with only small reserves of ecDNA survived bombardment from the drug, and once the drug was removed, they quickly made more circles, which propelled the tumor’s regrowth. Once again, the tumor was a conglomeration of cells with little to lots of ecDNA.
From any one cell’s perspective, ecDNA presents a trade-off between power and weakness. But for the tumor as a whole, it’s the best of both worlds: the perks of aggressive growth from cells stuffed to the brim with DNA circles, plus the safety net of cells that can get by with hardly any of the stuff. “That’s a pretty sweet deal for a tumor,” Mischel says.
And a pretty terrible deal for people with cancer.

Sequencing solutions
One reason circular DNA remained hidden in plain sight for so long is that scientists simply didn’t have good tools for finding them. Gene sequencing used to be clunkier, and our algorithms for interpreting genomic data weren’t trained to pick up on these circular tidbits.
Most sequencing technology relies on making several copies of the cancer genome and chopping them into short pieces that sequencing machines can easily read. Then, an algorithm lines up these DNA segments to a reference genome from a healthy human.
This process works well enough for the linear DNA on chromosomes. But circular DNA is a different story.
For instance, a sequencer might chop the hypothetical gene ABCDE into ABC and DE. But if ABCDE is on a circle, the start of the gene (A) touches the end of the gene (E). That poses a problem: the circle might be chopped up to create pieces—like EA—that don’t appear in the reference genome; the algorithm would see these as errors and discard them.
That shortcoming means we’ve been missing clues for ecDNA’s abundance for nearly 20 years.
Even though Mischel’s studies pointed to a role for ecDNA in glioblastoma, he didn’t have an easy way to figure out whether the phenomenon was also common in other kinds of cancer.
A few new tools have helped him, and others, answer that question.
Vineet Bafna, a computational scientist at UCSD who worked on the Human Genome Project, partnered with Mischel to develop software to detect and quantify ecDNA in microscope images of cancer cells. Bafna’s group has also written a program to search sequenced cancer genomes for clues that reveal the presence of circular DNA; a third program of his helps line up the genes on ecDNA in the right order.
Another key tool came from Birgitte Regenberg, a biologist at the University of Copenhagen, who discovered circular DNA in yeast in 2010. Her lab developed Circle-Seq, a method for physically isolating ecDNA from cells, removing any remaining linear DNA with enzymes, and sequencing the circular DNA that remains.
The groups have used their tools to demonstrate that circular DNA is much more common than their initial studies suggested. In 2015, Regenberg used Circle-Seq to discover more than 1,700 unique DNA circles in yeast, representing some 23% of its genome. And in 2017, Mischel and Bafna, using their image analysis and sequencing software, interrogated 2,500 cancer cells and found ecDNA in 40% of the tumor cell lines.
Mischel and Bafna’s studies provided an answer to a long-standing mystery about how cancer cells could multiply their genes so quickly. “We spent a lot of fruitless days trying to figure out the most simple and most clear explanation for changes in copy number,” Bafna says. The old sequencing techniques told scientists that gene amplifications were likely on chromosomes. Bafna and Mischel’s research suggests that ecDNA is likely the dominant way in which many cancers amplify genes. That discovery, Bafna says, was a “revelation.”
Some scientists, including Regenberg, are finding DNA circles in seemingly normal cells, although there’s much debate about their importance. These circles are often too small to contain a full gene, whereas ecDNA in cancer is large enough to carry multiple genes tied to tumor growth.
There’s even growing evidence that many organisms use DNA circles as a general strategy to steel themselves against things that should normally kill them. Yeast, the protozoan parasite Leishmania, and weeds all use DNA circles to resist toxic molecules, drugs, and herbicides, respectively, notes Jonathan Houseley, a Babraham Institute geneticist who studies ecDNA in yeast. “Circular DNA keeps popping up whenever we see resistance occurring.”

Circular DNA in context
Circular DNA offers a clean explanation for how tumor cells can acquire gene amplifications and drug resistance so quickly. But seemingly every time researchers try to unravel the mechanism by which ecDNA is created and operates, the story gets weirder.
The researchers who discovered double minutes in 1965 saw them in neuroblastoma, a rare nervous system tumor in children. Later, scientists found that these DNA circles sometimes carried amplifications of a cancer-promoting gene called MYCN. These MYCN amplifications are bad news for someone with cancer. And frustratingly, a portion of people with these amplifications have particularly aggressive tumors. Until recently, doctors couldn’t explain why.
Advertisement
It turns out that DNA circles don’t like to stay in one place. Anton Henssen, a pediatric oncologist at the Max Delbrück Center for Molecular Medicine, and Richard Koche of Memorial Sloan Kettering Cancer Center took a close look at ecDNA in neuroblastoma tumors and found that the circular DNA can sometimes slip back into chromosomes. In doing so, it can introduce new mutations and disrupt other genes. Henssen and Koche analyzed data from neuroblastoma patient samples and found that people with ecDNA had lower chances of survival, and the odds for those with DNA circles that had reintegrated into chromosomes were even worse.
Mischel and Bafna discovered a similar phenomenon in glioblastoma. When pressured with an EGFR inhibitor, circular DNA jumped back into chromosomes. This suggested that sometimes gene amplifications on chromosomes and gene amplifications in circles are intimately related. When the drug was removed, the chromosomes spat the DNA circles back out, and sometimes the circles would bring a new gene along with them.
The quirks of ecDNA didn’t stop there. We now know that ecDNA isn’t just a naked DNA double helix. Our cells organize DNA by wrapping it around proteins called histones. Keeping the wrapping tight turns genes off, and unspooling the DNA from the histones turns genes on. Mischel, Bafna, Roel Verhaak of the Jackson Laboratory, and Stanford University geneticist Howard Chang discovered that DNA circles are largely unspooled.
That helped explain another one of the team’s findings: the genes on DNA circles were among the most highly transcribed in the cancer genome. Cancer cells were using ecDNA to crank out enormous levels of RNA that in turn was used to make proteins that boosted the tumor’s growth.
Still, those discoveries didn’t fully explain why gene expression was so high. It turns out that DNA circles contain pieces of genetic code called enhancers, which are like loudspeakers for gene expression. Normally, an enhancer for one gene is kept far apart from the enhancer for another gene, but the circular shape of ecDNA places all the enhancers and genes close together. “There is a complete rewiring of the enhancer-gene interactions,” says Peter Scacheri of Case Western Reserve University, who discovered this rewiring with Jeremy Rich from UCSD.
Mischel’s team, as well as Henssen and Koche’s group, reported similar findings on enhancers. “This is one of those magical times in science where there are at least three independent groups that converge on the same concept,” Scacheri says.
Koche and Henssen say these discoveries are long overdue. When sequencing neuroblastoma tumors anew, they also found that circular DNA could now explain anomalies in data that had been discarded in previous experiments. “We will have a lot more to discover from mining previous data sets with circular DNA in mind,” Koche says. “I think it is going to be a very rich source that is currently untapped.”
In search of a target
At a recent investor meeting, Boundless Bio CEO Zachary Hornby presented results from an unpublished experiment. The company’s scientists treated a dish of cancer cells with a drug that targets a gene on ecDNA. Although circles bearing that gene declined, circles with another tumor-promoting gene soon popped up in their place. Trying to block the genes on these circles was like playing whack-a-mole. “This has big implications,” Hornby said. “It basically implies that a targeted therapeutic approach is not going to be effective in these types of patients.”
Drug developers have spent much of the past 2 decades designing compounds that selectively target proteins made from genes that are linked to cancer. But as Mischel’s glioblastoma research showed, this precision oncology approach doesn’t always work, particularly when trying to block proteins made by genes on DNA circles. Figuring out what to do about ecDNA may be even harder than studying it.
Since we still don’t know how the creation or reintegration of ecDNA is controlled, Henssen thinks the best strategy for drug developers might be targeting ecDNA-dependent cells indirectly. “The mere presence of ecDNA might make the cells behave differently than a cell that doesn’t have these circles floating around. And that different behavior might make the cell susceptible to certain therapies that wouldn’t harm normal tissue,” he says. “I am pretty confident that there will be mechanisms to be found.”
Boundless has dedicated itself to discovering those mechanisms. Hornby also doesn’t view ecDNA itself, or the cancer-promoting genes it carries, as the drug target. “We are not trying to directly bind ecDNA,” he says. “Rather, we are trying to inhibit the supportive machinery that ecDNA relies upon.” The team is going after three vulnerabilities: the enzymatic molecular machinery that supports ecDNA replication and transcription; the metabolic codependencies, which include the metabolic pathways that ecDNA-laden cells depend on to survive and thrive; and DNA damage-repair pathways.
“There are key proteins in each category that we are validating right now, or in some cases, we believe we have validated targets,” Hornby says.
The notion that ecDNA could create new strategies for treating cancer is beginning to get more attention. Henssen, Koche, and Scacheri all say they’ve been approached by venture capitalists and drug companies interested in ecDNA, although none of them have started a firm yet.
“I bet you if they come up with one drug that looks promising, it will start a revolution. But there are a lot of challenges,” Salk’s Wahl says.
“I think the field is going to explode,” Mischel says. “This is a biology that you can’t ignore.”



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter