Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Hope In A Pill
A crop of small-molecule drugs in development could double the treatment options for people with multiple sclerosis in coming years
by Lisa M. Jarvis
April 6, 2009
| A version of this story appeared in
Volume 87, Issue 14

IT WAS A SMALL INCIDENT, but it hit home. On a blustery February morning in New York City, a woman on the bus offered Rick Sommers her seat. She was getting off at the next stop, so it wasn't a big sacrifice, but for Sommers it had greater meaning. Nearly 15 years after being diagnosed with multiple sclerosis, a disease in which the immune system mysteriously wages war on the central nervous system (CNS), Sommers was for the first time using a cane.
"I've been fighting it for a long time," he says, "but I just know that the cane will give me sense of safety. If nothing else, it will alert people around me, 'Here comes a guy with a problem.' "
For Sommers, who learned he had MS not long after he finished his first marathon, carrying a mark of his disease is a tough adjustment. After all, in the unspoken etiquette of mass transit, giving up a seat is normally reserved for pregnant women and old folks. Although Sommers appreciated the passenger's graciousness, he thought, "I'm only 48 years old. This isn't right."
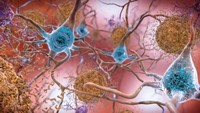
The cane is a sign that his disease is slowly worsening, despite more than a decade of treatment. MS can cause a host of physical and cognitive symptoms as the immune system attacks myelin, the protective coating on nerve cells. Sommers was diagnosed in 1994, when strategies to treat the disease were few and far between.
"Back then, there was one drug on the market," Sommers recalls. "It was an injectable called Betaseron, and I remember you had to be in a lottery to get on the drug." Sommers would get calls from the manufacturer asking whether he'd like to have his name thrown in the ring. He refused. "I was like, 'No, I'm not one of those people who are going to inject themselves.' "
Three years later, at the urging of his neurologist, Sommers became "one of those people." By then, Biogen Idec had introduced Avonex, a once-weekly version of interferon beta-1a, and he started what would become an 11-year hot-and-cold relationship with the drug: It helped his symptoms by reining in the immune system, but he dreaded the weekly shot and its flulike side effects.
Remarkably, the nearly 200 Americans diagnosed with MS each week do not have significantly different treatment options than Sommers did in the mid-1990s.
Take Blossom Beason, a 34-year-old who last summer started her own weekly ritual of Avonex injections after a series of magnetic resonance images (MRIs) and blood tests confirmed she has MS. Her doctor could only offer a choice between various beta-interferons, each with their pros and cons, and Teva Pharmaceutical's Copaxone, a synthetic peptide injected daily. The only new drug that has been introduced in recent years is Tysabri, a treatment from Biogen Idec that, because of risky side effects, is generally given only to people with progressive forms of the disease.
Worse, the available drugs seem to stop working at some point. A year ago, Sommers switched to Rebif—or as his neurologist calls it, "Turbo-Avonex"—because his mobility was starting to decline more rapidly. The sad truth is that even this amped-up drug may not be enough to delay further deterioration. Generally, people with MS live long lives but suffer physically and cognitively.

YET THERE IS HOPE for Sommers, Beason, and the roughly 400,000 Americans with MS. In the next few years, the treatment options could multiply as research efforts by major companies, including Novartis, Sanofi-Aventis, and Biogen Idec, start to bear fruit. The MS drug pipeline now boasts more than 10 treatments in late-stage clinical trials. In addition to adding to the weaponry in doctors' arsenals, many of the new drugs are pills rather than injectables. Most are small molecules that fine-tune how the immune system is modulated, whereas others aim to treat the symptoms of the disease by repairing some of the damage done to the CNS.
"It is a very exciting time," says Katherine Dawson, director of neurology at Biogen Idec. "For many years we had the interferons, then Copaxone, and more recently, after a break, Tysabri. All of a sudden, we have a whole bunch of drugs in development."
It remains to be seen whether these oral drugs are safer or more effective than existing therapies. After all, successfully modulating the immune system is a tricky business. The challenge has been to find the delicate balance between making the immune system less aggressive and not hobbling it so much that a person is more vulnerable to pathogens, says Bruno Musch, head of clinical development for neurodegenerative diseases at EMD Serono, the U.S. arm of Merck Serono.
Although none of the new drugs is a cure, "we have every reason to be excited about new medications," says Randall T. Schapiro, director of the Schapiro Center for Multiple Sclerosis, in Minneapolis. But Schapiro cautions that "just because it's oral doesn't mean that it's a smooth-acting, easy-to-take medication." All of these new drugs are potent, and clinical trials may show that the risks are not worth the benefits, he adds.
MS is a perplexing disease, and the cadre of potential new treatments is the culmination of years of research to better define it and understand how it progresses. Unlike, say, cancer, where a doctor can see a tumor, test for malignancy, and treat accordingly, MS is a challenge to detect and diagnose.
The symptoms of the disease include fatigue, numbness, depression, forgetfulness, and coordination and vision problems. Many could easily be mistaken for the results of a sports injury or be confused with the normal aches and pains of life. In Beason's case, her one "clinical episode"—numbness that started at her toes, spread to her waist, and lasted for two weeks—occurred some 10 years before a doctor considered conducting an MRI to check for the lesions on the brain that are the hallmark of MS.
Furthermore, MS progresses differently in different people. "If you talk to 10 people, you'll get 10 different stories on how they deal with their MS, what their symptoms are, what their treatments are," notes Sommers, who after years working as a radio DJ and comedian now counsels people with MS.
For decades, conflicting theories of the underlying cause of the disease were bandied about. Today, scientists think of MS as "an autoimmune disease of the CNS that occurs as a result of an environmental trigger happening early in the life of a genetically susceptible person," says John Richert, executive vice president for research and clinical programs for the National Multiple Sclerosis Society (NMSS). In other words, MS occurs when a person with a particular genetic makeup is in the wrong place at the wrong time.
Studies of MS clusters point to a range of potential environmental triggers, such as viruses and low levels of sunlight and vitamin D. They also suggest that the trigger needs to occur in a narrow window around the teenage years.
How the disease emerges after exposure to that trigger is up for debate. Although much research is still being done to figure out its underpinnings, one hypothesis is that MS is a case of molecular mimicry. A person is exposed to a virus adorned with proteins that are structurally similar to a myelin protein in the CNS. The immune system gets confused and attacks not only the virus but anything that looks like it, including the CNS protein, Richert explains.

The other dominant hypothesis is that the disease is simply a chronic infection. "In either case, the epidemiological data suggest that if there is an infection or infectious trigger, it is probably with a common virus that the body is exposed to, but people who are destined to develop MS are genetically programmed to respond to it in an abnormal manner," Richert says.
Until about 10 years ago, scientists thought MS was simply a problem of damaged myelin, the fatty layer that insulates axons, or nerve fibers, on a nerve cell. The prevailing idea was that the immune system attacks the myelin, causing nerve signals to fire less efficiently or leak out. The result is scar tissue, which shows up as lesions in an MRI.
But the advent of advanced confocal microscopy technology and antibody-based stains allowed closer study of the brain and spinal cord tissue of people with MS. Researchers realized that it wasn't just a problem of myelin. The axons themselves were also deteriorating.
THE DISCOVERY of axonal deterioration was a breakthrough. Scientists began to understand why the interferon drugs stop working for some patients. At a certain stage, the axonal degeneration becomes more prominent than the inflammation and demyelination, and the disease starts to behave less like an inflammatory disease and more like a neurodegenerative disease, such as Parkinson's or Alzheimer's.
That shift in understanding of the disease, along with improved information about inflammation pathways, has informed drug discovery efforts. The first crop of drugs, the beta-interferons, lacks finesse. Although beta-interferons, marketed by Biogen as Avonex, EMD Serono and Pfizer as Rebif, and Bayer as Betaseron, have helped many people with MS delay the progression of the disease, they are also indiscriminate in their methods. Beta-interferons bind to a receptor on T cells, which along with B cells are the main kinds of lymphocytes, or white blood cells, that make up the immune system's regulatory and maintenance team. Latching on to T cells slows immune response, but it also induces the expression of several hundred genes, many of which aren't related to the disease.
And because of that sweeping modulation of the immune system, the beta-interferons are marked by flulike side effects. During the first few months of treatment with Avonex, Beason learned just what flulike means. She experienced chills, fatigue, and fevers upward of 104 ºF. "The first month or so of having the full dose was not fun," she says.
The new small-molecule drugs incorporate a more refined understanding of the immune system. "The whole goal of these new immune therapies is to try and get as specific as we can to the disease at hand, as opposed to globally suppressing the immune system," says Shreeram Aradhye, global clinical franchise head for immunology and infectious diseases at Novartis.
At the same time, many of the small molecules in development are first or second cousins of earlier compounds that were rejected, primarily because of unattractive side effects. Still, companies think they've ironed out the quirks of the predecessor drugs while they get a better understanding of how they work.
They are taking a range of approaches. Novartis is tapping into the potential of a derivative of myriocin, a product naturally found in a fungus that had been used for thousands of years in Chinese medicine. The company is trying to block the surface cell proteins that guide lymphocytes out of the lymph nodes, according to Volker Brinkmann, a research project leader at Novartis.
Once activated in the lymphatic system, T cells and other immune cells travel the busy highway known as the bloodstream to get to their target tissues. Nature has provided them with a built-in GPS: proteins that sit on the surface of the cells and point them to the proper exit ramps during their journey. In the early 1990s, scientists realized they might be able to alter the course of the disease by disabling that GPS.
NMSS subsequently gave its first grant to study the effects of blocking alpha-4-beta-1 integrin, a protein that tells immune cells when to leave the bloodstream and enter the brain and spinal cord. "If you could block that, maybe you could prevent immune cells from getting in and doing damage in MS," Richert explains.
The resulting product is Biogen's Tysabri, a humanized monoclonal antibody that has proven highly effective in keeping MS from progressing. In fact, it works in some 70% of people with MS, a significant improvement over the beta-interferons.
Novartis' lead drug in development for MS, fingolimod, binds to another surface cell protein, sphingosine-1-phosphate (S1P) receptor, which tells the immune cell to leave the lymph nodes. As a result, some T cells are kept out of circulation, where they can later stir up trouble in the nervous system. According to Brinkmann, fingolimod can also reach the CNS, meaning it could also reduce neurodegeneration.
Advertisement
SO FAR, fingolimod has proven highly effective in clinical trials. In a large Phase III study comparing it with once-weekly beta-inteferons, fingolimod reduced relapse rates by 52%, Aradhye notes. Beta-interferons, meanwhile, reduce rates by only about 30%.
But blocking those exit ramps can have a downside. Drugs like Tysabri keep the immune system from going in and stripping the myelin from nerve cells, but they also keep the immune system from fighting legitimate infections in the brain and spinal cord. In early 2005, just months after its launch, Tysabri was taken off the market after Biogen learned of two deaths from progressive multifocal leukoencephalopathy, a rare brain infection typically seen in people who have severely compromised immune systems, such as AIDS patients. The drug returned to the market in the fall of 2006, but anyone taking it is carefully monitored for signs of the brain infection.
Because Tysabri is so effective, some people with MS, primarily those whose disease has progressed despite treatment with the beta-interferons or Copaxone, are willing to take the risk. Others, such as Sommers, see Tysabri as a last resort.
Since fingolimod has a similar mode of action as Tysabri, albeit blocking a different exit ramp, conventional wisdom would suggest caution. "There are some risks, of course, in altering the migration behavior, which is why we are planning this large clinical program," Novartis' Aradhye explains.
Indeed, seven cases of localized skin cancer occurred in the fingolimod branch of a clinical trial, compared with one case in the interferon branch. The cause has yet to be determined, but given the problems with Tysabri, the news gave researchers pause. The MS community is now anxiously awaiting more clinical trial results for fingolimod, expected to be made public at a neurology meeting in late April. Analysts are forecasting a 2010 launch for the drug.
Although Novartis' highly targeted drug is at an advanced stage of testing, industry-watchers expect that the first small-molecule MS drugs to reach the market will, like the beta-interferons and Copaxone before them, take a more global approach to treating the disease. For example, rather than carefully modulating the immune system, EMD Serono's cladribine suppresses lymphocytes entirely.
Cladribine, a purine nucleoside, was first developed at the Scripps Clinic, in La Jolla, Calif., where doctors used it to treat a rare form of leukemia in which B cells have gone awry. The drug is given to cancer patients either intravenously or by injection, but it was reformulated for oral administration for MS patients.
"The whole goal of these new immune therapies is to try and get as specific as we can to the disease at hand, as opposed to globally suppressing the immune system."
TREATING MS with a drug that has worked on cancer is not a new approach. EMD Serono also markets Novantrone, a cytotoxic agent that knocks out the activity of T cells, B cells, and macrophages. It is an aggressive way to treat MS and one that doctors resort to only when the disease is worsening despite treatment with other drugs. They administer Novantrone by intravenous infusion once every three months and limit the overall amount given in a patient's lifetime because of risk of heart attacks and a form of leukemia.
Like most chemotherapies, cladribine is more akin to a sledgehammer than a surgical strike. However, it also appears to be a kinder, gentler cytotoxic drug. Cladribine is given less frequently than Novantrone and at a very low dose: A person takes the pills just four or five days for one week per month, two months in a row out of the year. "The lymphocytes go down and stay down," Musch says. By the end of the year, their levels have crept back up, and the two-month treatment cycle starts anew.
Cladribine could therefore find a broader audience than Novantrone, possibly even as a first line of attack for the disease. EMD Serono plans to file a New Drug Application with U.S. and European regulatory agencies at midyear. The drug will be fast-tracked by the Food & Drug Administration, meaning it is poised for a 2010 launch.
Still, EMD Serono recently reported that four cases of malignancy surfaced out of 1,000 patients treated with the drug in a Phase III study. "It's too early to say whether this is important or not, but certainly, it is something everyone is keeping an eye on," NMSS's Richert says.
Some neurologists caution that even if cladribine turns out to be effective, they would be hesitant to prescribe it to women with mild forms of the disease. "Any drug that is a chemotherapeutic you don't want to give to a woman of childbearing years," because it could cause fetal abnormalities, notes Robert P. Lisak, chair of neurology at the Wayne State University School of Medicine, in Detroit.
Lisak has similar concerns about another cytotoxic agent in development: teriflunomide, Sanofi-Aventis' lead MS compound. However, Stefan Schwabe, Sanofi's vice president for CNS neurology projects, says teriflunomide differs by modulating the growth and activity of lymphocytes without completely suppressing their function. Lymphocytes are "still circulating and moving around, still making contact with B cells," he notes.
Teriflunomide is the active metabolite of leflunomide, a drug Sanofi sells under the brand name Arava to treat rheumatoid arthritis. Leflunomide is metabolized to teriflunomide in the liver, and Sanofi scientists posited that circumventing that step would also circumvent some cases of liver damage seen with Arava.
THE DRUG BLOCKS dihydroorotate dehydrogenase, a critical enzyme in pyrimidine synthesis. Because activated lymphocytes rely on pyrimidine for survival, the theory is that T-cell function will be dampened by knocking out the enzyme. The key, Schwabe notes, is that some immune system pathways are preserved, meaning the body hasn't totally lost its defense mechanisms.
Two other drugs in development appear—so far—to have the cleanest safety profiles, which means they could have mass appeal if they can just match the efficacy of existing injectable treatments. Teva's laquinimod and Biogen's BG-12 are neck and neck in the race to market, and both have long legacies in the research world.
Laquinimod is derived from roquinimex, a quinoline carboxamide that had shown modest activity in MS before Pharmacia & Upjohn Inc. halted its development in 1997 after a Phase III study suggested it increased the risk of heart attack.
Researchers at the Swedish firm Active Biotech thought there was still life left in the approach and generated more than 60 quinoline-3-carboxamide derivatives to try to engineer out the cardiovascular concerns. After testing those compounds in an animal model, the company determined the quinoline ring controls how well the drug works, whereas the N-carboxamide substitution dictates side effects. Laquinimod had the best balance of efficacy and safety, and in 2004, Teva licensed it.
"A lot of work was done to improve the safety profile of the product," and that safety has been demonstrated in late-stage trials, says Rivka Riven Kreitman, head of innovative R&D at Teva.
The mechanism of action, however, is still unclear. "We are still investigating how it works," Kreitman notes. Animal studies have shown that the drug does not keep the immune system from mounting an attack, which means it is not acting as a broad immunosuppressant. Data suggest that the drug is acting as an immunomodulator, but the company is continuing to study its effect.
Biogen Idec's most advanced MS molecule, which seems to have a winning combination of safety and, in Phase II trials, efficacy, also has a long history. In the 1950s, Biogen's Dawson explains, German and Swiss doctors found that fumaric acid esters were an effective topical treatment for psoriasis, and for years patients would simply go to a compounding pharmacist and have a salve mixed. Decades later, a company called Fumapharm decided to explore a systemic treatment. It launched an oral psoriasis product, Fumaderm, in Germany in 1994.
Fast-forward to just a few years ago, when a German neurologist contemplated the link between MS and psoriasis, which at the time was thought to be a T-cell-mediated disease. He decided to try the Fumapharm drug on his patients, and in 2006, he published data showing it was having an impact on lesions seen on brain scans.
Fumaderm, however, was not an ideal treatment for a chronic disease. It causes flushing and some unpleasant gastrointestinal side effects. Fumapharm began developing fumaric acid derivatives that maximized efficacy while minimizing side effects. It eventually hit upon dimethyl fumarate.
Biogen teamed up with Fumapharm to develop the drug, now known as BG-12, and eventually acquired the company. As the clinical program progressed, Biogen has been able to apply its years of knowledge about MS to get to the bottom of how the drug works.
Although Dawson cautions that research continues, it appears that BG-12 turns on the Nrf2 transcriptional pathway, which is responsible for protecting the blood-brain barrier and defending axons and neurons against oxidative stress. As a result, BG-12 seems not only to dampen the inflammatory process but also to be neuroprotective.
Advertisement
Working backward, the company has confirmed the hunch of the German neurologist who first experimented with fumaric acid. "We see that there does seem to be a real rationale that this agent is effective for this particular disease," Dawson says. "That is very exciting, and we're looking in Phase III trials to try to document the neuroprotection," a feature that other drugs in the pipeline wouldn't offer.
"If you talk to 10 people, you'll get 10 different stories on how they deal with their MS."
Although Biogen is first developing the drug as a treatment for earlier stages of MS, the potential neuroprotective effect could be useful in treating people whose disease is in the later stages, in which neurodegeneration is taking over. "What we've recognized in the past couple of years is that axonal loss probably occurs very early in the disease," Dawson says. Thus, even when inflammatory activity dominates during the early stages of the disease, the drug would still be useful to protect axons and neurons.
OTHER COMPANIES have developed small molecules that specifically target the CNS. The rationale is that by providing chemical insulation for demyelinated nerve fibers, these drugs would help people with MS treat the symptoms of their disease for the first time.
Acorda Therapeutics is developing a potassium-ion-channel blocker that improves conduction in demyelinated nerve fibers. Excitability in the brain is controlled by two kinds of currents: Potassium ions act as the brake, and sodium and calcium ions as the accelerator. The trick to Acorda's drug, fampridine, is blocking enough potassium channels to improve conduction of nerve impulses without inhibiting their function so much that sodium and calcium ions send the brain into overdrive, explains Andrew R. Blight, Acorda's chief scientific officer.
Late-stage trials of fampridine showed that people with MS were able to walk faster than could those taking a placebo. Acorda recently filed a New Drug Application with FDA.
Sanofi is also trying to insulate axons. Nerispirdine, in Phase II trials, blocks both potassium and sodium channels. "This is a very exciting way to go forward," Sanofi's Schwabe notes. Although scientists have yet to prove that neuroprotection will have a long-term effect on the course of the disease, "we do see that if you somehow maintain the function of the nervous system, you can also maintain its structure," he says.
Furthermore, the neuroprotective molecules can be used in conjunction with the immunomodulatory drugs. "The response for fampridine is the same in people who take an immunomodulator or not," Blight notes. This could be good news for someone like Sommers, who is having mobility problems despite taking Rebif.
For people with MS, oral drugs that could address both the immune and neurological components of the disease represent a beacon of hope. "If I could take a pill, I almost wouldn't mind having this disease," Sommers says. Mentally gearing up for the weekly shot and the possible side effects takes its toll over the years, he says. Putting aside the syringes "would make it a lot more tolerable," he says. "I am very excited that there might be some oral drugs down the road."






Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter