Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Taking Aim At Brain Tumors
Nanomedicine: Gold spheres decorated with RNA block cancer gene expression in mice
by Bethany Halford
November 4, 2013
| A version of this story appeared in
Volume 91, Issue 44

Scientists have created a new weapon to test in the fight against the deadly brain cancer glioblastoma multiforme. By packing strands of small interfering ribonucleic acid, or siRNA, onto the surfaces of gold nanoparticles, they made a nanomedicine that entered the brains of mice and then slipped into tumor cells. There, the siRNA neutralized genes that make those cells flourish.

“Glioblastoma multiforme is one of the worst cancers one can get,” says Chad A. Mirkin, a chemistry professor at Northwestern University who helped invent the cancer-fighting nanoparticles. The disease kills approximately 13,000 people in the U.S. each year, and life expectancy once diagnosed is 14 to 16 months. Doctors currently treat the disease by surgically removing the tumor, followed by radiation and chemotherapy. But this aggressive approach extends life expectancy by only a few months.
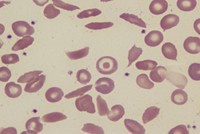
The team led by Mirkin and his colleague Alexander H. Stegh thought it might have a better method for fighting this tenacious cancer. In 1996, Mirkin developed spherical nucleic acids, or SNAs, which are nanoparticles covered with either DNA or RNA. The nucleic acids in turn can interact with genes and proteins. SNAs have been used for medical diagnostic tests and as topical medicines. In 2007, Stegh and coworkers identified a gene that is overexpressed in glioblastoma tumors. Mirkin and Stegh decided to build an SNA equipped with siRNA that is capable of interfering with that gene, a process known as RNA interference (RNAi).
When injected into the bloodstream of mice with glioblastoma multiforme, the SNA nanoparticles travel through the body. About 1% of them cross the blood-brain barrier, the barricade that protects the brain from toxic agents. The nanoparticles accumulate in tumors, rather than healthy brain tissue, because they are trapped in the tumors’ unusually distorted blood vessels. The researchers found that treatment shrank tumors and increased the survival rates of the mice. Unlike other therapies based on RNAi, no other agent was required to deliver the RNA (Sci. Transl. Med. 2013, DOI: 10.1126/scitranslmed.3006839).
“The RNAi approach shown here has huge potential,” comments Omid C. Farokhzad, a nanomedicine expert at Harvard Medical School. “The effectiveness of SNAs for uptake into cells makes them uniquely suitable for RNAi applications.”
“Crossing the blood-brain barrier with an siRNA-based approach that does not involve a separate pharmacological agent to open the blood-brain barrier is significant,” adds John J. Rossi, an RNAi expert at the Beckman Research Institute of City of Hope, a cancer center in Duarte, Calif. “The SNA approach could be applied to neurological diseases such as Alzheimer’s or Parkinson’s, using different siRNAs specific for those diseases.”
AuraSense Therapeutics, a company cofounded by Mirkin, has licensed the technology. The next step, the researchers say, is to do safety and efficacy studies in primates. They hope to begin human clinical trials by the end of 2014.






Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter