Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Polymers
New materials take a bite out of tooth decay
Mercury and gold give way to polymer composites, alternative cavity treatments, and new tooth replacement materials
by Marc S. Reisch
August 1, 2016
| A version of this story appeared in
Volume 94, Issue 31

Many people walk around with a mouthful of mercury-containing fillings and have no problems with them at all. But if they think about it, they might wonder why a material with a reputation for toxicity is lodged in their teeth.
To be clear, regulators at the U.S. Food & Drug Administration and the European Union continue to vouch for the safety of dental amalgams, which are about half mercury and half a mix of other metals including silver, tin, and copper. A standard treatment for about 160 years, amalgam fillings are an effective and low-cost fix that can last 20 years or more.
But mercury-filled thermometers and thermostats disappeared from store shelves long ago because of environmental concerns surrounding the element. And now mercury-containing amalgams could be on their way out as international pressure builds to cut back on their use.
Cavity conundrum
The two major dental filling types have pros and cons
▸ Low price
▸ Easy to placer
▸ Lasts 15 to 20 years
▸ Wears down slowly
▸ Dark gray appearance
▸ High price
▸ Difficult to place
▸ Lasts seven to 10 years
▸ Wears down more quickly
▸ Tooth-colored
Sources: FDA, American Dental Association, industry interviews
To replace amalgams, dental material companies are offering newer materials and treatments. These include polymeric composites to plug cavities, treatments to stop tooth decay in its tracks, and peptides to alter the microbiome in a person’s mouth and prevent decay from happening.
Technological advances are also leading to new materials that replace teeth that are beyond repair. Gold in crowns and bridges is being replaced by less costly zirconium oxide, polyether ether ketone, and lithium disilicate glass-ceramic materials. Three-dimensional printers and computer-guided lathes are using these materials to shape dentures, bridges, and crowns.
Bye-bye, amalgams
Behind the move to limit use of mercury is the 2013 Minamata Convention on Mercury. Signed by the U.S. and 127 other countries, the treaty calls for restricting mercury in the environment, where it breaks down into methyl mercury and other toxic forms of the element.
Mercury goes down the drain when dentists drill into amalgam-containing cavities, explains John E. Dodes, a dentist who practiced in New York City for 45 years and is an authority on the safety of amalgams. Mercury vapors are also released during drilling. Still, mercury emissions from dentistry are dwarfed by those from other sources, including coal-fired power plants and gold refining, he says.
According to the United Nations Environment Programme, coal burning accounts for 24% of global mercury emissions and gold refining for 37%. UNEP has not quantified emissions from disposal of dental amalgams.
The composites that are replacing mercury amalgams have been around since the 1960s, but have their problems too. Some release small amounts of bisphenol A, an endocrine disrupting chemical, Dodes says.

According to the American Dental Association, BPA is not used directly as an ingredient in dental materials, but it is used to make monomers such as bisphenol A-dimethacrylate (bis-DMA) and bisphenol A-diglycidyl ether methacrylate (bis-GMA) that are found in dental composite resins. Any BPA that comes from these chemicals would be at trace levels that are unlikely to be a health concern, it says.
Such concerns, whether over amalgams or newer composites, are to be expected when replacing one of nature’s most refined products. “Tooth enamel and dentin naturally in your mouth are perfect materials; everything after that is inferior,” says Alan Boghosian, a Chicago dentist with 36 years of clinical experience.
As Dodes sees it, amalgam fillings are not a danger to patients, are easy to place, and cost 30 to 70% less than composites. Also, the silver in the fillings oxidizes over time, helping prevent further decay. But an amalgam filling “is not pretty,” he admits, because it turns dark gray. “In my opinion, amalgam is the filling of choice if there is no cosmetic reason to place a white composite filling,” he says.
Composite makers do in fact tout the “aesthetic” benefits of the tooth-filling materials. Methacrylic-based composites, which are reinforced with inorganic fillers such as silica, ceramic, and zirconium oxide, are formulated to look translucent just like real teeth, says George Tysowsky, senior vice president of technology at Ivoclar Vivadent, a dental materials formulator.
Composite materials are being adopted as the dental industry moves away from amalgam fillings. The amount of mercury sold in the U.S. for dental amalgams in 2013 was 14,500 kg, half what it was in 2001, according to a survey released at the end of last year. The data comes from the Interstate Mercury Education & Reduction Clearinghouse, a confederation of states dedicated to the phaseout of mercury.
How to make a better filling
Ivoclar has made strides, according to Tysowsky, in developing composite filling materials that cure faster and perform better. Composite fillings are more difficult to work with than amalgams, which naturally expand into a cavity. Most polymer composites use a photoinitiator to cure. After placing a thin layer of composite in a cavity, a dentist uses a blue LED light to cross-link and harden the polymer matrix.

But if the composite isn’t evenly exposed to the light, or the light can’t penetrate it, the cure will be less than ideal and could fail over time, Tysowsky says. To fix the problem, Ivoclar developed a composite that works with an improved germanium-based photoinitiator and light exposure system.
Most other dentistry initiators, such as camphorquinone and trimethylbenzoyl diphenylphosphine oxide, cure only to a depth of about 2 mm, Tysowsky says. But Ivoclar’s germanium-based photoinitiator, together with a more powerful LED light, cures to 4 mm deep, allowing a more complete cure in less time than other composite systems, he says. The average cavity is 3 to 6 mm deep.
Every dimethacrylate composite shrinks as it cures, points out Andrew Ritts, regulatory affairs director at Nanova Biomaterials, a start-up firm. “But with fillers they shrink less, and fiber reinforcement reduces the shrinkage even more.” Nanova reinforces its acrylic-based composites with fillers such as silica plus a nanofiber made from hydroxyapatite, a type of calcium phosphate that is similar to bone.
The fiber, unique to Nanova, was developed by University of Missouri mechanical engineering professor Hao Li, who is also president of the firm. FDA cleared Nanova’s fiber-containing composite last year. “We make the fiber ourselves,” Ritts explains.
Although Ritts suggests the firm’s filling material will last at least as long as other composites—about seven to 10 years—a great deal depends on dental placement technique. Dental professionals say this is true of just about all composite fillings and a reason why installing them is generally more expensive than amalgam fillings.
Going beyond fillings
Some dental professionals want to go beyond fillings, be they amalgams or composites. “Repairing cavities like repairing potholes is ridiculous,” says Boghosian, who is also a professor in the dental surgery division of Northwestern University’s Feinberg School of Medicine. “We need biocompatible materials, and we need to get the body to make more of what it makes. That would be the best way to replace tooth structure.”
Researchers are already working on ways to get teeth to repair themselves. Scientists at the University of Nottingham and Harvard University’s Wyss Institute are developing a biomaterial they say can be used like any other dental filling. Placed in contact with tooth pulp tissue, it can stimulate native stem cells to regenerate the pulp and surrounding dentin.
Although scientists involved in the research say they aren’t ready to identify the materials they have developed, Adam Celiz, a research fellow at Nottingham, tells C&EN that the light-curable materials are “purely synthetic” and degrade over time as the body repairs the tooth.
Celiz and others on the project recently won a $4,000 prize in the Royal Society of Chemistry’s Emerging Technologies Competition for the research. Commercial development, Celiz says, will follow publication in a scientific journal.
While researchers advance the self-repairing tooth technology, others are harnessing a cavity-arresting alternative that has been used in Japan for more than 80 years. Treatment with silver diamine fluoride (SDF), according to Peter Milgrom, an oral health professor at the University of Washington, stops cavities in their tracks.
Milgrom says he learned of the treatment years ago and convinced FDA to clear it in 2014. Elevate Oral Care sells his formula as Advantage Arrest.
Very young children, elderly people, and the disabled often can’t endure or sit still long enough to allow a dentist to drill and fill a cavity, Milgrom explains. A dentist using Advantage Arrest merely has to paint less than a drop of the formulation on a cavity. As it penetrates tooth enamel and dentin, the silver kills off bacteria that promote tooth decay, and the fluoride helps remineralize the tooth, he says.
Although the cavity is still present, the treatment, which should be repeated every six months, effectively arrests the decay, Milgrom says. One drawback is that the silver turns the cavity a grayish black color.
Also, in about 10% of cases, the treatment seems to be ineffective, Milgrom notes, probably because not enough solution made it onto the cavity. “We’ve added a blue color to the SDF so the clinician can see where they are putting the treatment,” he says.
Researchers are also exploring the use of peptides that might prevent decay from starting. In the June 2015 issue of the Proceedings of the National Academy of Science (DOI: 10.1073/pnas.1506207112), Wenyuan Shi, a professor at the University of California, Los Angeles, and colleagues explain how an antimicrobial peptide could wipe out acid-producing Streptococcus mutans bacteria, the main cause of tooth decay, without disturbing the beneficial bacteria in the mouth.
Shi’s Los Angeles-based firm, C3 Jian, has raised more than $100 million to advance the decay-preventing peptide, dubbed C16G2, and other peptide products. Now in Phase II clinical trials, C16G2 would be formulated as a mouthwash. If it succeeds, the peptide could put a significant dent in the more than $100 billion spent annually in the U.S. on dental services, the firm claims.
New teeth? No problem

When teeth are beyond repair and have to be replaced, glass-ceramics, polymers, and low-cost metals are replacing high-priced metals.
Gold- and palladium-based metals have traditionally been used for crowns, dentures, and bridges. In crowns, for instance, porcelain fused to gold has been the benchmark for both performance and tooth appearance.
But the high cost of porcelain/gold crowns and porcelain’s tendency to chip are providing an incentive to develop more cost-effective materials, Ivoclar’s Tysowsky says. One alternative is a lithium disilicate (LDS) glass-ceramic crown and tooth material for dentures and bridges.
One advantage of LDS, Tysowsky notes, is a crystalline structure that makes it durable. The coloration, opalescence, and translucence of the material, for which Ivoclar has the original patents, makes it hard to distinguish from a natural tooth.
Another alternate material for replacement teeth is zirconium oxide, which is even stronger than LDS, according to Tysowsky. The material performs well and is resistant to fracturing, he says, but doesn’t have the optical properties of LDS.
New materials such as LDS and zirconium are becoming popular not only because they appear more like a patient’s own teeth, but because solid blanks can be milled into patient-customized dental structures on computerized equipment.
Another material that can be machine milled is the engineering polymer polyether ether ketone (PEEK). “Some people have allergies to the metals used to make dental frameworks,” explains Marc Knebel, medical segment director for the specialty chemical maker Evonik Industries. His firm markets PEEK, which has been available to dental labs only in the past four years. It is biocompatible, is resistant to body fluids, and doesn’t leach residual monomer, he says.
However, PEEK is not what Knebel would call an “aesthetic material” because it doesn’t have the translucent appearance of a tooth. So it is more likely to play a supporting role, for instance in crowns, where it could be covered with a composite coating for a more toothlike appearance.
Fashioning PEEK and other materials in computer-guided equipment is revolutionary, says Dodes, the New York dentist. Many dentists are beginning to order dental crowns and frameworks made with the new machines.
“Most of the crowns I made in the last five years started with traditional impressions that were then digitally scanned at a dental lab by lasers and milled in computer-guided machinery,” he says. “They fit beautifully.” The milling method replaces the lost-wax technique used to cast gold and other metals for dental appliances.
Advertisement
“Good casters using the lost-wax technique are hard to find today, and they are expensive,” says Ed Littlewood, dental products marketing manager for the 3-D printer and scanning equipment maker Renishaw. Moreover, computer-aided milling and printing are more precise and less fraught with quality problems, he says.
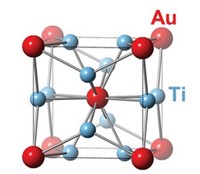
The 3-D printers made by Renishaw use the “powder bed fusion technique,” in which successive thin layers of a powdered metal such as a cobalt-chrome alloy or titanium are fused by a laser, Littlewood says.
Renishaw’s 3-D printers are now available to U.S. dental labs and the firm is setting up centers to demonstrate them. “This technique is growing rapidly now, but not as rapidly as it will grow in the next few years,” Littlewood predicts.
Given the materials, production methods, and treatments available today, dentists can offer patients a variety of handsome, durable, and economical treatments. “There is a sweet spot for every individual,” says Boghosian, the Chicago dentist. Synthetic materials will never live up to natural enamel and dentin, but they are coming closer.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter