Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Biological Chemistry
Antibody disrupts blood-brain barrier
Found in people with an autoimmune disease, the antibody could give researchers clues about delivering drugs to the brain
by Michael Torrice
July 10, 2017
| A version of this story appeared in
Volume 95, Issue 28
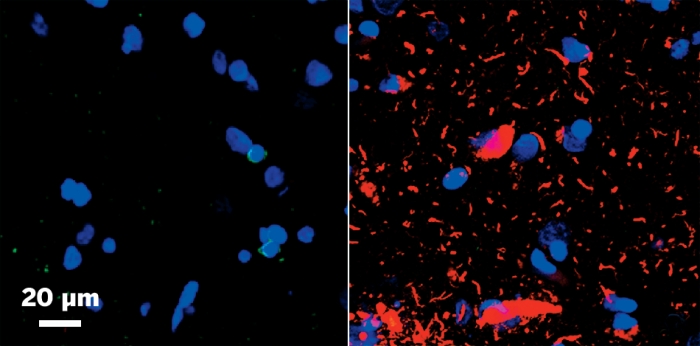
Cells along the blood vessels in the brain form tight junctions to prevent toxic molecules—and often drug molecules—from entering the brain. Researchers have found an antibody that disrupts this blood-brain barrier in some people with an autoimmune disease (Sci. Transl. Med. 2017, DOI: 10.1126/scitranslmed.aai9111). The findings could lead to strategies to deliver drugs to the brain, the researchers say. Neuromyelitis optica is an autoimmune disease in which the immune system attacks a certain protein in brain cells, often leading to inflammation and damage to the optic nerve and spinal cord. Antibodies targeting this protein can get past the blood-brain barrier, so scientists wondered how they performed the feat. A team led by Richard M. Ransohoff of Biogen and Jeffrey L. Bennett of the University of Colorado School of Medicine found that another antibody in patients’ blood can bind to and activate the endothelial cells responsible for forming the barrier. The team determined that this antibody targeted glucose-regulated protein 78 (GRP78) on the cells’ surfaces. Injecting the GRP78 antibody into mice daily for seven days increased the permeability of the animals’ blood-brain barriers, allowing proteins of different sizes to leak into the brain from the blood. Disrupting the blood-brain barrier for drug delivery is fraught with neurotoxicity issues, says William A. Banks of the University of Washington and VA Puget Sound Health Care System. But, he says, this study’s findings give scientists a new player to study to better understand the regulation of this important interface between the blood and brain.




Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter