Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Toxicology
Big tobacco embraces in vitro toxicology
Manufacturers invest in nonanimal tests to evaluate health risks of e-cigarettes and other next-generation tobacco products
by Britt E. Erickson
October 28, 2018
| A version of this story appeared in
Volume 96, Issue 43

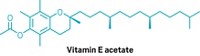
Toxicology tests that rely on human cells and tissues instead of animals are rapidly evolving, driven by widespread interest in reducing the cost and stigma associated with animal testing and the desire to test large numbers of chemicals rapidly. Now, tobacco firms are joining pharmaceutical, pesticide, and chemical manufacturers in investing heavily in the technology.
Big tobacco is making more appearances at scientific conferences focused on nonanimal toxicology testing. Representatives from tobacco giants—British American Tobacco, Japan Tobacco, Philip Morris International, and Reynolds American—participated in the annual meeting of the American Society for Cellular & Computational Toxicology (ASCCT) in September. Their ultimate goal: to convince officials at the U.S. Food & Drug Administration’s Center for Tobacco Products (CTP) that in vitro methods for predicting respiratory toxicology in humans are ready for prime time.
The industry is facing increased testing requirements for e-cigarettes and other tobacco products that entered the market after Feb. 15, 2007. That’s the date set by the U.S. Congress when it gave FDA authority to regulate tobacco products in 2009. The law exempts tobacco products that were on the market as of the 2007 cutoff date from the requirements. Most e-cigarettes, however, hit the U.S. market after that date.
In 2016, FDA deemed e-cigarettes to be tobacco products, so manufacturers of e-cigarettes, and the tens of thousands of different flavored e-liquids used with them, are required to register their products with FDA. Initially, manufacturers were supposed to file these premarket tobacco applications by Nov. 8 of this year for tobacco products released between 2007 and August 2016. Now they have until Aug. 8, 2022. The extension gives FDA more time to finalize the guidelines and industry more time to generate the necessary data. But manufacturers of products that hit the U.S. market after August 2016 need to register their products with FDA right away, before they put them on the market.
As part of registration, companies must provide information related to known health risks of the product, as well as a list of the components and ingredients in the product and how the product is used.
FDA is trying to keep up with the latest science, but the agency has yet to finalize guidelines for industry regarding what information is sufficient to show that new tobacco products are appropriate for protecting public health. That standard is much different from the one FDA uses to approve new drugs, which manufacturers must show are safe and effective.
The public health standard requires manufacturers to assess the risks of a new tobacco product on the entire population, including potential impacts of the product on smoking cessation as well as smoking initiation, particularly in youth.
Milestones in the oversight of U.S. tobacco products
2009: Tobacco Control Act becomes law. The Family Smoking Prevention & Tobacco Control Act gives the U.S. Food & Drug Administration authority to regulate tobacco products. The law exempts tobacco products that were on the market before Feb. 15, 2007.
2016: FDA issues draft guidance for e-cigarettes. FDA releases preliminary guidance regarding toxicity testing and other information necessary to demonstrate that electronic nicotine delivery systems are “appropriate for the protection of the public health.” FDA also finalizes its rule deeming e-cigarettes to be tobacco products.
2022: Certain regulatory submissions are due. The deadline for manufacturers of e-cigarettes and other next-generation tobacco products to submit applications for FDA authorization is Aug. 8, 2022. This deadline applies only to products that entered the market between 2007 and August 2016. Manufacturers of tobacco products released after Aug. 8, 2016, must receive FDA authorization before they can legally sell their products in the U.S.
The tobacco industry claims that the lack of regulatory guidance on how to meet the public health standard is leading to a delay in the development of new products that are less harmful than conventional cigarettes, such as “heat not burn” cigarettes, also called heated cigarettes. These cigarettes, which are currently unavailable in the U.S., contain tobacco that is heated to a much lower temperature (up to 350 °C) than conventional cigarettes (more than 900 °C). Manufacturers say the levels of harmful chemicals in the heated cigarette vapor are lower than those from a traditional cigarette. On a risk continuum, heat-not-burn cigarettes would fall somewhere between conventional cigarettes and e-cigarettes, independent experts say.
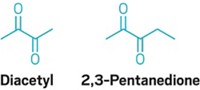
The complexity of next-generation tobacco products has increased by a number of factors since FDA was given responsibility to regulate tobacco, Phil Yeager, supervisory toxicologist at CTP, said at the ASCCT meeting. In addition to more than 10,000 e-liquid flavors, each of which FDA considers a separate tobacco product, e-cigarettes come in many variations, he said. Additionally, e-cigarettes have no long-term epidemiological data, so evaluating chronic exposure is difficult, he said.
Tobacco companies hope in vitro tests that use human lung cells or tissues will be sufficient to show that their new tobacco products, including e-cigarettes, significantly reduce harm and disease and benefit the population as a whole when compared with traditional cigarettes. Several of them are working with independent, third-party laboratories to standardize in vitro assays for respiratory toxicology so that results from one lab can be easily compared with results from another.
Much of the work involves comparing the levels of hazardous chemicals in traditional cigarette smoke with those in e-cigarette vapor. Manufacturers say that they are not trying to show that e-cigarettes and other new tobacco products are safe but rather that they pose a lower risk to human health than cigarettes.
Conducting such testing with animals is “not practical, economically or otherwise,” says Holger Behrsing, principal scientist at the Institute for In Vitro Sciences (IIVS), a nonprofit organization that offers in vitro toxicology testing services to numerous industries, including cosmetics and personal care products, pharmaceuticals, and tobacco. The organization receives funding from these industries to support outreach and education initiatives. “Animal tests really are not that accurate,” he adds. “Within respiratory toxicology, that is especially true.”
Behrsing is head of a newly constructed respiratory toxicology lab that opened in 2017 at IIVS. The facility is equipped with a special heating, ventilation, and air-conditioning system that allows scientists to control the temperature and humidity in the lab. This control is important for testing tobacco products because standardized tests for reference tobacco cigarettes require cigarettes to be conditioned at 60% humidity and 22 °C before testing, Behrsing says.
IIVS scientists use human donor tissues, obtained from organs that are not suitable for human transplants, to create cell cultures and in vitro test systems. In some cases, they use precision-cut lung slices to test for inhalation hazards. They also use human donor stem cells from companies such as MatTek and Epithelix that can be propagated and reconstructed into a 3-D tissuelike airway. “We refer to those as reconstructed airway tissues,” Behrsing says.
Thanks to a donation last year from the PETA International Science Consortium, an advocacy group that promotes nonanimal toxicology testing, IIVS is also now home to a $100,000 commercially available smoking machine made by Vitrocell Systems. The system generates airborne materials from test products, such as smoke from reference cigarettes and vapor from e-cigarettes, in a manner that simulates how a person would puff.
Scientists expose human lung cells or tissues to the airborne material generated by the machine to mimic inhalation exposure. They can then evaluate changes such as fluctuation of protein mediators of inflammation known as cytokines, altered gene expression, or cell death.
IIVS scientists have developed assays to look at additional end points, such as effects on tiny, hairlike structures called cilia that protrude from cell surfaces. “Our upper airways have cilia that are constantly beating” to help the lungs remove inhaled material, Behrsing says. Using microscopy and video-analysis software to quantify how quickly cilia beat, the scientists can then look at the effect on cilia of exposing reconstructed airway tissues to cigarette smoke or vapor.
“When you smoke tobacco, it actually increases cilia beating for a little bit,” Behrsing says. The cilia work harder to remove irritants in the smoke from the lungs. But eventually, the cilia’s beating goes back down, he says. In time, chronic exposure to tobacco smoke can lead to dysfunction of the cilia and impaired clearance of mucus.
IIVS scientists use reconstructed airway tissues from stem cells for these experiments because the approach allows them to easily see the beating cilia. But the reconstructed airways have only four or five types of lung cells, while lung slices contain all of the more than 40 cell types found in lung tissue, Behrsing says.
The researchers are working to standardize the cilia beating assay as well as two other assays involving lung cell mucus production that may predict chronic obstructive pulmonary disease. IIVS is collaborating with several tobacco companies, tissue vendors, and FDA’s National Center for Toxicological Research to compare results from the different organizations.
The IIVS scientists, along with others in the field of respiratory toxicology, are grappling with whether it is better to expose tissues to smoke or aerosol generated by a smoking machine or to liquid extracts of the smoke or aerosol captured onto and eluted from filter pads. The extracts make it possible to quantify components in the smoke, such as nicotine, that are deposited on the tissues. But extracts don’t contain all the materials that are in smoke, just what is caught on the filter pad, Behrsing says.
Researchers know that e-cigarette aerosols generated by smoking machines vary from one machine to another. So it is difficult to compare results unless scientists can quantify the amount of each test substance delivered to cell cultures. “It is really important to understand how the aerosol is generated, how it is potentially diluted, and how it is delivered to the cell culture systems,” Marianna Gaca, preclinical assessment manager at British American Tobacco, said at the ASCCT meeting. She emphasized the importance of in vitro dosimetry—the determination of the dose delivered to cellular systems in vitro.
Advertisement
Large tobacco companies are using a wide array of in vitro assays of varying complexity, Gaca noted. British American Tobacco, for example, uses simple cytotoxicity assays with human lung cells to screen large numbers of e-liquids for potential health effects. Such screening helps companies decide which chemicals to include in their products, Gaca said.
Not all e-liquids currently available to consumers, however, have been through any safety testing, never mind meeting the to-be-determined requirements for FDA authorization. “You’ve got a lot of small mom and pops that are coming up with these flavors, and they probably don’t have the budgets to be putting together the big safety packages,” Erin Hill, president of IIVS, says. When the four-year grace period is up, experts predict that many of these small manufacturers will either go out of business or risk illegally selling products that FDA considers adulterated.
“The big tobacco companies that are working in the space of course do put in a lot of screening and assessment of these flavors,” Hill notes. “But what they are going to have to do is standardize those approaches,” she says.
Standardization is key to regulatory acceptance, Hill says. “That is a big role that we play at IIVS—standardizing approaches so that the regulatory agency has confidence in them,” she adds. “We’ve done that with the U.S. EPA around antimicrobial cleaning products, and we are working in the pesticide area,” she says. “It has to be done in order for a regulatory agency to be able to accept these new approaches.”
Regulating e-cigarettes as over-the-counter drugs
Manufacturers of tobacco products intended for recreational use, including e-cigarettes and other electronic nicotine delivery systems, must meet a high bar to get a new product onto the U.S. market. Products developed after Aug. 8, 2016, have to obtain U.S. Food & Drug Administration authorization before they can be legally sold in the U.S. Products already on the market as of that date have until August 2022 to obtain FDA authorization.
“FDA is working out the kinks right now” on the authorization process and what data to require in those premarket tobacco applications, says Azim Chowdhury, a partner at the law firm Keller & Heckman. “But it is going to be very onerous,” he tells C&EN. “It is going to be a potential deal breaker for most of the industry.”
The challenge for tobacco product manufacturers is that they must meet what’s known as the public health standard, which requires manufacturers to assess the potential risks of their product on the population as a whole rather than just the individual user. For e-cigarettes and other new tobacco products, this means manufacturers must demonstrate to FDA that their new product will not increase overall tobacco use or initiation and will not decrease cessation of tobacco use, Chowdhury says.
In draft guidance for premarket tobacco applications for recreational use, FDA recommends that manufacturers submit data from nonclinical, clinical, and long-term studies to meet the public health standard. E-cigarette manufacturers are weighing the pros and cons of registering their products as recreational tobacco products. The alternative is to go through the new-drug approval process, which requires companies to show FDA that e-cigarettes and other new tobacco products are safe and effective for promoting smoking cessation or treating tobacco addiction.
Meeting FDA’s standard for drug safety and effectiveness would require quite a bit of data, Chowdhury says. “But it may ultimately be easier than meeting the public health standard,” he adds.
This is particularly true if FDA creates an over-the-counter (OTC) drug pathway to demonstrate e-cigarette safety and effectiveness. By classifying e-cigarettes and other tobacco products as OTC drugs, FDA could review a large number of similar products as one category rather than assess each one individually. But FDA would first have to create a standard called an OTC monograph that it would use to compare products against. For example, FDA could create one monograph for all e-liquids using a standardized e-liquid to demonstrate an end point such as smoking cessation or treatment of tobacco addiction.
It remains to be seen whether FDA will create an OTC drug pathway for e-cigarettes. It is also unclear how much data would be required from manufacturers if FDA does create such a pathway. “Generally, OTC status comes from products that have a long history of use,” Chowdhury says. “We don’t have that history with these products. They’ve only been on the market about 10 years, so it is going to take quite a bit of work.”



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter