Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Pharmaceuticals
Covid-19
Podcast: Diagnose, treat, vaccinate—beating a killer coronavirus
Stereo Chemistry looks at lessons learned from previous epidemics and the global effort underway to stop this new microscopic foe
by Megha Satyanarayana
May 1, 2020
| A version of this story appeared in
Volume 98, Issue 17

As COVID-19 continues to spread, so does the effort to find treatments for and vaccinations against SARS-CoV-2, the coronavirus that causes the disease. Around the world, scientists are working nonstop on therapies they hope will stem the loss of life during this pandemic while trying to set us up to prevent future outbreaks. What’s not clear is which of these treatments will work. Much about SARS-CoV-2 remains unknown. In this episode of Stereo Chemistry, we dig into the efforts to beat the novel coronavirus and why in some cases it’s like throwing spaghetti against the wall to see what sticks.
Subscribe to Stereo Chemistry now on Apple Podcasts, Google Play, or Spotify.
The following is the transcript for the podcast. We have edited the interviews within for length and clarity.
Support nonprofit science journalism
C&EN has made this story and all of its coverage of the coronavirus epidemic freely available during the outbreak to keep the public informed. To support us:
Donate Join Subscribe
Tedros Adhanom Ghebreyesus: WHO has been assessing this outbreak around the clock and we are deeply concerned both by the alarming levels of spread and severity, and by the alarming levels of inaction. We have therefore made the assessment that COVID-19 can be characterized as a pandemic.
Matt Davenport: Hey, everyone. Welcome to Stereo Chemistry. This is Matt Davenport, and I hope you’re all keeping safe and healthy. Who you just heard was Tedros Ghebreyesus, the director of the World Health Organization. And in this clip from March, he officially classifies the outbreak of a novel coronavirus as a pandemic.
Today, we’ll be talking about this coronavirus that has many of us isolated in our homes. But even though I’m isolated, I am not alone. In fact, we have a very special cohost today. Thank you for joining us, Megha.
Megha Satyanarayana: Hey, Matt. How’s it all going?
Matt: Good. I mean, it’s been tough at times. But overall, we’re good, and everyone in our house is healthy. And my daughter got to meet yours over Zoom, which was very, very cool. How about you? How’s everything going?
Megha: Yeah, that Zoom meet was super adorable. So I live in Dallas, which is one of the cities that has had large numbers of cases of COVID-19. This is the name that’s been given to the respiratory disease that the novel coronavirus, SARS-CoV-2, causes. So we’ve been doing our best to keep busy, keep working, and to stay at home as much as possible.
Matt: So before we dive in, I want to say that I’m really excited that you’re back on the podcast. You did an amazing bonus episode earlier this year, but because this is your first full episode, would you mind if I asked you to introduce yourself?
Megha: Thank you. Of course. Hi, everyone. I’m Megha Satyanarayana. I’m sheltering here in place in Texas. And at C&EN, I cover both the biological side of chemistry as well as the pharma and biotech industries.
Matt: Awesome. And just one last piece of bookkeeping before we get going on today’s topic. Megha and the team at C&EN have been reporting around the clock as this pandemic evolves to bring you the most current and accurate information possible. But obviously, this is a very fluid situation.
What we’re going to do with this podcast today is paint you a broad-strokes picture about therapeutic development when any new pathogen emerges, then highlight examples of that for this coronavirus. But we’ve also got up-to-the-minute news about the virus online at cenm.ag/coronavirus. And all of that news is freely available during this pandemic.
OK, so, Megha, I know this is a big ask, but could you maybe set us up with everything we need to know about this virus so we can talk about how we’re starting to fight it?
Megha: I’ll certainly try. So in the fourish months since we first learned about a strange pneumonia and its ties to a seafood market in China, there has been this massive global scientific effort to try and teach us what this virus is, to teach us what its proteins do, to figure out how it gets inside cells, what possible drug targets it might have, and how we might vaccinate against it.
And so now there are now hundreds of drug trials going on and several vaccines in clinical trials. And some of these trials are beginning to yield results, which means that, if all goes well, by summer, we could potentially have some drugs for treating this disease. Vaccines will take longer, and we’ll go into that in a minute.
But believe it or not, this is all still very fast. And I think this is because of two things. In terms of biology, what we already know about two related coronaviruses, the SARS coronavirus and the MERS coronavirus, has helped streamline a lot of the work that’s gone into what we understand about SARS-CoV-2. And in terms of developing the tools we need to fight it, what we’ve learned from Ebola outbreaks and how science and industry approach drug and vaccine development during these periods of rapid and deadly infection have also helped.
Matt: OK, so it’s April 28, the day that we’re recording. Let’s talk about where we are today. Do you mind if I fire off a few basic questions?
Megha: Fire away.
Matt: How many people have died from COVID-19?
Megha: More than 200,000 people have died.
Matt: And how many confirmed cases have there been?
Megha: Worldwide, we’re now well over 3 million. And it’s important to note that these numbers, the number of people who’ve died and the numbers of people who have had positive tests, these are all underestimates. There have been a lot of problems with testing and the accurate reporting of cases. And this is something that we’ve been covering, so I’ll just remind you all that the place you can go to see all this reporting is cenm.ag/coronavirus.
Matt: And for today, I think one of the big questions is how many treatments do we have for this disease?
Megha: Right now, Matt, the fair answer is zero. None.
But honestly, as we’ve been recording this episode, data are starting to come in from Phase III trials of a drug called remdesivir. And we’ll talk a little bit more about that later. So like you said earlier, it’s a fluid situation, and things could change in the not-too-distant future. Right now, if you end up in the hospital with COVID-19, you are treated with what’s called supportive care, which I think you’ve heard of if you’ve heard of stories about ventilators and things like that. But is there a definitive pill? Is there a sure-fire injection? Not yet. No.
That being said, there are a lot of chemical strategies that are in the works that will hopefully protect us from this virus down the line. There are a lot of drugs that have been developed for other uses that are now being tested against this coronavirus. And at the same time this is all going on, new molecules are being developed.
So right now our best weapon against this virus, as you know, is social distancing. Staying at home. You know, Matt, we’ve talked a lot about flattening the curve. And what this really is doing is buying time. It’s buying time for our health-care systems to make sure that hospitals are not overwhelmed with large numbers of sick people all at once. And at the same time, it’s also buying time for the people who are developing the diagnostics, the treatments, and the vaccines to really be able to roll something out that will help us stay healthy in the long term in the face of this infectious disease.
Matt: That really brings us to why you and I are here today. To talk about what the scientists are doing with that time and how they fight pandemics.
But I do have one more fundamental question that I think we should spend some time on, which is what do we know about the biochemistry of this virus? And how does knowing help researchers develop these tools that we’re wanting to fight it with?
Megha: Yeah, I love this question. So, in order to fight a pathogen, it’s helpful to understand what it is and how it infects. Very quickly, within weeks of the first reports of this weird pneumonia, scientists in China had sequenced the virus’s genome, which is made of RNA rather than DNA. DNA being what the human genome is made of.
A pathogen’s genome is an important starting block for many reasons. For one, we can develop diagnostics. For viruses, what this means is something that’s based on a method called PCR, polymerase chain reaction. In this assay, what you take is a patient’s sample, and you are looking for the tiniest traces of viral genetic information that’s hidden among all of the human genetic information.
And so, in this assay, what happens is that viral genetic information, which is RNA, gets converted to DNA. That DNA get amplified, and then, every time it gets amplified, a little tag is added to it. And that allows it to be read out in a way that gives you an indirect answer: “Yes, you have viral RNA in your body.” But it’s not a direct reading; it’s not cultured virus from that person.
So while it’s a useful test in determining who might be in the middle of active infection, it’s not really a yes or no. Many people will test positive for viral RNA long after their last symptom. But are they still producing and shedding virus? Are they still infectious? These are still some of the big questions that are out there.
That being said, these tests were really successful in helping places like South Korea stem the tide of disease, because they were able to deploy widespread testing. A person who tested positive for viral RNA could be isolated, and their contacts could be traced, and the spread of the disease could be slowed down. On the other hand, in the United States, we’ve had a lot of problems with developing these tests and rolling them out really quickly. And so we’re, unfortunately, we’re really quite behind the curve.
Matt: So what I’m hearing is having the virus’s RNA sequence is a big deal, but it’s not in itself enough.
Megha: It’s essential, but it’s not sufficient. So keep that in mind as we start talking about therapies and vaccines, as well.
Matt: And should we talk about those now?
Megha: Sure. So having the sequence of this virus also allows us to develop diagnostics, but it also allows us to begin to understand the proteins that make up SARS-CoV-2. There are 29 of them. And some of them will end up becoming drug targets. And we can start doing the structural biology that helps chemists and biologists do drug discovery and vaccine development.
You’ll remember me saying that the first SARS coronavirus and the MERS coronavirus are related to this novel coronavirus. They’re all cousins. They share a lot of genetic information. And they’ve all jumped the species barrier from animals to humans. So they also share some aspects of that host-pathogen interaction that leads to infection and disease. All of this has given researchers a head start in their efforts to understand and hopefully stop SARS-CoV-2.
Matt: But we don’t have an approved vaccine for SARS or MERS yet, right? Is it wrong for me to be a little incredulous about how much they can help us fight SARS-CoV-2?
Megha: So the reasons why we don’t have an approved vaccine for these other viruses don’t necessarily have anything to do with the virus itself or the virus’s biochemistry. It really just has more to do with how the course of infections has gone and how that’s affected the development of vaccine and testing.
Advertisement
So if you think about this, since 2005, the number of global MERS infections has been about 2,500. The SARS outbreak was about 17 years ago, and about 8,100 people were diagnosed with the disease. About 30 countries were involved. And there were a small number of cases in the US, and then the virus just kind of petered out. And so the need for vaccines maybe hasn’t been as urgent because the disease has not been as widespread.
SARS-CoV-2 is totally different. I mean, we’ve got more than 3 million confirmed cases across nearly every country in the world. So the outbreaks, the spread of disease, have been quite different, but the viruses are similar.
I imagine you’ve probably seen a lot of images of coronavirus out there, that it’s like a little sphere with these little knobbly things all over the surface. Those knobbly things represent something called the spike protein.
And that spike protein is what helps the virus get inside our cells. And in the case of SARS and the MERS coronavirus, it turns out they’re vaccine targets. And for SARS-CoV-2, guess what? Also a vaccine target.
Jason McLellan: And if we look at people that have been infected with SARS, for instance, or MERS, the overwhelming amounts of antibodies that humans make is directed against the spike protein. And so we want to use that information to develop spike-based vaccine antigens and allow the human body to recognize it.
Megha: That was Jason McLellan. He’s a structural biologist at the University of Texas, Austin. His team revealed the structure of the spike protein of the novel coronavirus, SARS-CoV-2. And that work is actually informing one of the leading vaccine candidates against the disease, which is being developed by Moderna in conjunction with the National Institutes of Health.
Matt: So we have a target, but it’s part of a deadly pathogen. How do we get it into a vaccine that sort of presents it to our immune systems safely?
Megha: So there’s a conventional way to make vaccines, and this is also going on with SARS-CoV-2. You take a viral protein, and you can put it in a nonpathogenic virus. That virus infects you, and it causes an immune response, but you don’t get sick.
Or you could use a weakened or a deactivated SARS-CoV-2 virus. The virus has all of its proteins, but, again, it’s not going to make you sick. It’s just going to elicit that immune response that will hopefully be remembered if you ever are infected by the actual infectious, virulent SARS-CoV-2. So these are the more traditional ways that you build a vaccine.
But at the same time that these traditional vaccines are being developed, there are some new technologies out there that people are working on to try and get these viral proteins in front of our immune systems a little faster. Because those proteins are what prompts our immune system to act.
And one way of doing that is by taking the genetic instructions for the spike protein instead of the protein itself and putting those into biomolecules—and those genetic instructions can be messenger RNA or they can be the DNA that corresponds to that RNA—and then using that as the basis of a vaccine. Here’s Jason again.
Jason McLellan: The alternative method is to create molecules, either mRNA, DNA-based vaccines, or viral vectors that can be injected into a person’s muscle. And then their cells, their own cells, take that genetic information and produce spike protein and either secrete it or put it on the surface of the cells. And then the body recognizes that spike protein is foreign and raises antibodies. And that can be done really quickly.
Matt: How quickly?
Megha: So do you remember the company I just mentioned, Moderna? Moderna actually had an mRNA-based vaccine candidate already in development for another coronavirus. So once we had the structure for the SARS-CoV-2 spike, the company was able to work with the National Institutes of Health to get a vaccine candidate into Phase I trials in 6 weeks.
Anthony Fauci, who’s the director of the National Institute of Allergy and Infectious Diseases—which is the part of the NIH leading this work—said that this is the fastest that anyone has gone from a genetic sequence to a Phase I trial for a vaccine.
But I will say that there are some things you really can’t rush. At the same time that Fauci was telling Congress back in March about this 6-week speed record to Phase I, he was also telling them that it will be almost a year and a half before we will have a fully vetted vaccine.
Matt: So, I don’t want to sound ungrateful, but sitting here, right now, 18 months sounds like an eternity. Why does it take so long?
Megha: You don’t sound ungrateful, and that’s a really good question. I’m going to turn this over to Joan Nichols, who is an infectious disease researcher and the associate director of the Galveston National Laboratory to try and explain.
Joan Nichols: Why does it take time? It takes time because you have to go through that process that says, first, we test it in the lab, we make it, and make sure that it functions. Then we put it in animals, make sure it’s not toxic to an organism. Are there any issues we catch at the point when it’s in preclinical testing? And then it has to go on testing in small groups of people before it gets out there. And that’s why it’s going to take a year or a year and a half, or maybe a couple years to get one. It’s not going to be quick.
Megha: So you have to remember that these trials are testing whether this vaccine works or not. So one possible outcome is it works and it’s great. The other possible outcome is, of course, that it doesn’t. There are no guarantees there
So one thing that I think is worth mentioning is that vaccines may not protect everyone. I spoke with Warner Greene about this. He’s an infectious disease expert who runs the Gladstone Center for HIV Cure Research.
He told me by way of comparison that with some of the HIV vaccine candidates, efficacy ranges from about 30–40%. And what he says is that, for coronavirus, we need that efficacy to be a little bit higher because of how the disease spreads comparatively.
But the same time, people are recovering from COVID-19, which means that hopefully they’ve developed antibodies against the virus. And so maybe these people will be protected. We still don’t really know.
So even if that vaccine isn’t 100%, you’re still helping build a larger population of people, hopefully, that are protected. Joan Nichols sort of draws this relationship based on the H1N1 outbreak of 2009. Here she is again.
Joan Nichols: This virus is here now, it’s going to stay with us. I don’t know how many people remember 2009 when the influenza that was a novel influenza that came into our population. It stayed with us through the next couple years.
We have more and more people that have recovered and are protected naturally, and we kick in with a vaccine and we protect some of the people that didn’t get infected that we need to protect, this virus will slowly cause less and less problem in our population, just like the flu does every year.
Megha: And this is why testing remains important. As countries start talking about opening themselves back up, as states are ending lock downs, health experts are reminding us that we still need to know who has been infected and who has not. But also we need to know who among the healthy people have been infected and recovered, and by turn who might be still susceptible.
So like we mentioned earlier, some countries have done a good job with this. And in the US, we’ve had some early stumbles. So as testing is starting to become more available in a couple of senses, hopefully that will change.
For instance, many companies are producing millions and millions of these PCR-based tests that will hopefully reach more people. And the FDA just approved an at-home test for use in the United States.
So, in the meantime, on top of these tests that look for genetic material, there are also these blood tests that measure the immune response by looking for the presence of antibodies against the novel coronavirus. And there are also tests in development that look for presence of viral proteins in the blood. These blood tests can be used for diagnosis, but really they’re good for tracking, for understanding who might have already had this infection.
Matt: And watching the news about testing, I think it’s a reminder that even though we have the science to do them, it’s not a guarantee that everything is going to go right. For example, we’re still seeing stories about possible reagents shortages for tests, as well as people saying we just don’t know how well these tests work. How many false negatives, how many false positives are they giving?
Advertisement
Megha: Yeah, I mean, in this pandemic we’ve already seen the supply chain get sorely tested when it comes to diagnostics. We’ve seen a lot of problems with logistics. But another huge issue has been validation of the diagnostics themselves. This virus is spreading really rapidly and these tests are getting developed very quickly, and so it’s hard to know how well they’re going to perform in the field compared to how they’ve performed in lab test.
Again, this is why we are social distancing ourselves. This is why we’re trying to flatten the curve by staying at home. Because, remember, as we talked about before, we’re also trying to buy time to make sure what we’re putting out there actually does work, whether it’s tests or pharmaceutical treatments for COVID-19.
Matt: Speaking of which, is it time we started talking about those potential treatments?
Megha: Yes. Right after this short break.
Matt: So, still Matt. And I just wanted a minute to say that I think now’s a really good time to subscribe to our newsletter. And I know that sounds super self-promotional, but there’s more to it than that. We’re all going through this pandemic together and there’s a lot we don’t know. We’re doing our best to bring you all the coronavirus news you need to stay current and you’ll find that in the newsletter. But our newsletter is also a great way to stay current with our quote unquote regular coverage. You know, hardcore chemical science, policy, and business. And, personally, that has helped me stay a little bit grounded during this time. Chemists are making news every day and you’ll read about that in our newsletter. Whether its because they’re developing treatments to a novel virus, or urging officials to address PFAS pollution, or because they’ve made a ridiculously huge molecule, our newsletter will help you stay connected. So if you aren’t already subscribed and would like to be, head over to cenm.ag/newsletter to sign up. Thanks a lot.
Megha: So we’re back. Before the break we were talking about vaccine development and how long it can take.
Matt: And I’m still feeling really conflicted about that. I mean, on the one hand, I’m excited that we went from a virus sequence to a vaccine trial in six weeks. But waiting 18 months for the trials to wrap, that’s some cause for angst.
And so I’ll just come out and ask what’s weighing on me heaviest, which is any drug or therapy is going to have to be tested against coronavirus with clinical trials, right? Does that mean we’re talking months or years before we have any medicine that helps?
Megha: I mean, it’s hard to say. So the good news is that there are a lot of therapies in clinical trials right now. Some of the data is going to start trickling in between now and the summer. But there is no guarantee that any of it will work. Failure is a huge part of science in that way.
So that being said, we’re not starting from scratch. As is the case with vaccines, past outbreaks inform how chemists develop novel drug candidates for this new coronavirus. And, of course, we’re learning more and more about how the virus infects and how cause disease each day. So what that means is that we’re finding new ways to think about fighting it, as well as more opportunities to try and use existing drugs that have already been through clinical trials for other diseases. That clinical data is still helpful.
And don’t forget that people are also recovering from this disease. We can capitalize on what we gather from their immune responses to help other people. So there are reasons for optimism.
Matt: And you know how much I love optimism. But I do have one more sourpuss question for you. Given all that, it sounds like developing a totally new drug is not the way to go in a pandemic. Is that true?
Megha: So it’s not that we shouldn’t develop new drugs, it’s that it takes many years to develop them and to test a new compound or biologic. So it’s faster to see if something already out there might have an effect based on what we know about the pathogen and the disease and related pathogens and the disease they cause.
So I think it’s fair to say that it’s still too early to speculate on which candidates might be the most promising, but there are some out there being developed as we speak. So you shouldn’t be too surprised if a new drug or a new biologic helps us control this disease in the future.
Matt: OK. So let’s talk about some of those existing drugs, drugs that are already approved. Chloroquine has to be the most famous, but not necessarily for the best reasons.
Megha: So in late March,we had a pretty comprehensive story about efforts to use those antimalarial drugs for Covid-19. What I’ll say here is that testing of chloroquine and hydroxychloroquine for treating SARS-CoV-2 isn’t there yet. It hasn’t happened at a large enough scale to give any truly meaningful results. Small tests have been inconclusive, others have been stopped. And one thing I should point out is that these are pretty harsh drugs. Some hospitals have been using it experimentally and they’ve stopped because the side effects have just been too hard on their patients.
Matt: So you mentioned that chloroquine is a malaria drug.
Megha: Yes. It’s also used to treat lupus.
Matt: Right. So it makes sense that we’re sort of looking at everything that’s already approved in our arsenal to fight this virus. But I’m wondering if maybe there’s something out there that might be a bit more obvious to someone like me, like something that actually fights the symptoms of the disease, rather than the virus itself.
Megha: Oh, that is definitely something people are looking at. Before we jump in though, do you know what happens when you get infected with a virus?
Matt: Not in a real scientific sense.
Megha: So, briefly, when a virus meets a human cell, it fuses with our cell membrane and the virus dumps its genetic payload inside that cell. And then it gets the cell to turn that information into more viruses that then pop out and go onto infect more cells. While all this is going on, the cell that’s infected is crying “mayday, mayday, help.” And this mayday sets off the immune system.
However, one of the vicious outcomes of this, in some people, is what’s been called cytokine storm, which is kind of when your immune system just goes bonkers while doing its job. With this coronavirus, that overdrive more or less destroys a person’s lungs, and potentially other organs too. The lung effect is called ARDS—acute respiratory distress syndrome—and it seems to be one of the main thing that is killing people who have COVID-19.
Matt: Gotcha. So if you could find a drug that’s already designed to control our immune response, or at least prevent it from going bonkers, that would be a good thing.
Megha: Yes. There are a bunch of drugs that deal with inflammation and immune overdrive in diseases like arthritis and those are now being tested for COVID-19.
Matt: That sounds straightforward.
Megha: It’s not. We need to understand how to use those drugs in a way that dampens the immune overreaction but doesn’t turn it off entirely. There’s a balance there. Because we still need those immune cells to kill the virus. If we dampen down the immune response too much, then the virus will get a better foothold. So there are ongoing trials that are attempting to try and solve this problem. Here’s coronavirus expert Lisa Gralinski from the University of North Carolina.
Lisa Gralinski: The NIH has been studying ARDS and trying to prevent this for decades now, but it’s incredibly complicated. So it’s a really fine balance. We’ve done some work with that in our lab looking at SARS pathogenesis. And so far, we’ve mostly found a lot of ways where you can make mice more sick. So I think that’s going to be a delicate balance to require a lot of testing and kind of a careful assessment of what’s happening in each person’s response to infection before just throwing drugs at people.
Matt: All right. I’m picking up on a theme here. We need more time. We need more experiments. We need more trials.
But I wondered if we could switch gears from that and go over something that I’ve heard is being used now, which is convalescent plasma.
Advertisement
Megha: Sure. Convalescent plasma.
Matt: So my question has two parts. One, what is it? And two, is that true? Is it something we’re actually using right now?
Megha: OK. I’ll start with part one first. If I get infected with coronavirus—let me knock on wood really quickly—and I recover, it will be because my body develops antibodies to help me fight off this infection. The idea is that these antibodies, my antibodies, could also help other people fight off their infection. And so to get the antibodies from me, I would donate my plasma. That’s the clear part of your blood that settles to the top of the tube when you have a blood draw at the doctor’s office. That plasma could then be transfused to another patient and my antibodies could hopefully help them.
Matt: OK. That makes sense and I’ll remind you of part two again. This is a thing we’re doing now question mark.
Megha: Yes. Papers about treating patients with plasma started coming out of China in March. And, as of now, several hundred people have received convalescent plasma in the United States. And one thing to point out is that this is actually early 20th century medicine. Here’s Warner Greene again.
Warner Greene: So this has been used as far back as during the time of the Spanish flu. It’s been used in the case of the Ebola outbreak and actually isolating antibodies from such a recovering individual led ultimately to a monoclonal antibody that joins another one that is actually a fantastic therapy for Ebola. If delivered early, these two monoclonal antibodies can essentially cure people who normally would have died.
So antibody therapy is certainly real. Of course, it only lasts as long as the antibody is present. And so you might have to re-infuse or continue to deliver the antibody, and that’s why the ultimate solution is a vaccine.
Megha: So yes, convalescent plasma is being used now. But it’s not your be-all, end-all solution.
Matt: OK. And can I check one other thing? Warner mentioned that natural antibody helped develop a therapy. Might we see something similar here where the natural antibodies could help researchers sort of design drugs for this virus?
Megha: Yes. Yes, that’s happening with coronavirus. We could definitely see trials of engineered antibodies that are based on the natural antibodies as early as this summer.
And I want to point out another part of his comment that’s really important. Earlier we talked about what we’ve learned from MERS and SARS and how that’s been important to our SARS-CoV-2 response. I want to take a minute to talk about how other infectious disease outbreaks have also taught us crucial lessons that we are making use of now.
So during the Ebola outbreak in West Africa between roughly 2013 and 2016, there were a lot of hurdles to getting clinical trials off the ground, and one of the end results was that some of these trials really only started only as the outbreak was waning. This made it, of course, hard to get the numbers that you needed to have really significant results in trial, to really be able to really tell if your drug or your vaccine was working.
And so the questions that were being raised during that outbreak were as straightforward as, should we even do research in the middle of a crisis, where healthcare workers are stretched and the medical system is breaking down? Or questions like, if we say that the only reasonable way to test if the drug works is during an outbreak, then can we morally do a randomized trial? Shouldn’t everyone be getting the drug and should no one be getting the placebo if they’re infected?
And so the WHO created a set of guidelines about how to conduct a clinical trial under these circumstances. And the guidelines, it’s a long list, but some of the things that they stress are things like having good efficacy data in non-human primates. Making sure that health systems are not going to be overburdened by the effort of your trial. And to really make sure that people really understand the risks of getting the treatment, which, as you know, is the basis of informed consent.
So what that meant was that a lot of trials, including for vaccines, started or continued during the next Ebola epidemic in the Democratic Republic of Congo. That outbreak started just started a couple of years ago and by the end of 2019, we saw vaccines getting approval.
Matt: So these are some of the experiences, then, that are informing clinical trials for COVID-19?
Megha: Yeah, I think so. So collectively, I think anytime that there is an outbreak, I think there are lessons that can be learned. For example, speed. Clinical trials are not always fast–they take months to years, depending upon the treatment, the ability to enroll people, how often people have to take the medication, the spacing between doses, how long patients are being tracked, all of this matters.
And there’s one last thing I want to talk about that we’ve gained from our efforts against Ebola and, believe it or not, that’s a drug candidate.
Matt: For the coronavirus?
Megha: Yeah, it’s called remdesivir and it was developed by a company called Gilead during an outbreak of Ebola in West Africa a few years ago. So the safety trials that they did on that drug during the previous outbreak has actually allowed researchers from China and the NIH to move straight through to Phase 3 trials of the drug for use against coronavirus. That started in February. And Gilead itself began enrolling patients in its own Phase 3 trials in March. And again, as we’ve been recording this podcast, results are starting to come out from those trials. What we’re learning at this stage is remdesivir is not going to magically cure disease in everyone and it’s not going to prevent it from spreading. And Gilead will also face challenges scaling up the production of the drug. That being said, the data are promising, Remdesivir seems to reduce the amount of time that the sickest people end up spending in the hospital, they get to go home sooner. And it’s expected that the Food and Drug Administration will issue what’s called an Emergency Use Authorization that would make the drug more readily available.
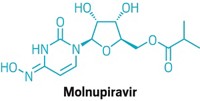
Matt: So how does it work?
Megha: So remdesivir is an antiviral. And what it does is it sort of outfoxes the enzyme that’s responsible for building virus’s genetic code piece by piece. This enzyme is called polymerase and in coronaviruses, what it does, is it normally detects and repairs mistakes as it builds up the viral RNA sequence.
So as the polymerase is building the viral RNA sequence, remdesivir can sneak in and the polymerase can’t tell that it’s a mistake. So now what you have is a virus that can’t replicate itself. It can’t make proteins.
So it turns out that remdesivir wasn’t as good a treatment for Ebola as some of the other treatments involving something called monoclonal antibodies. But, again, because Gilead tested it during these Ebola outbreaks, we know already that it’s fairly safe in humans. And that’s saving us a little bit of time in terms of trials, so now we can go to efficacy trials.
Here’s Sina Bavari, who is now a consultant but previously worked on infectious disease response at the US Army Medical [Research] Institute of Infectious Diseases. He gave me an idea of how much time this would take for a new drug.
Sina Bavari: In a typical scenario, from the start of looking at antivirals to the time you go into clinic, it could take more than a year to about a year.
Matt: Dang. We are much less than a year into this, which is really exciting. But I am waiting for the other shoe to drop.
Megha: So remember that we’re in the middle of a pandemic. Because of that science is happening sort of out of order. Remdesivir is being tested in people, but we don’t have the depth of preclinical testing that we normally would going into those human tests. So for example, the NIH has just released some data from a study in monkeys earlier this month, showing that remdesivir did slow the progression of COVID-19 in those animals. And Lisa Gralinski has told me that they are ramping up to try and test remdesivir on SARS-CoV-2 infected mice.
So another thing to think about is that clinical trials during outbreaks are often designed without placebo arms. If you remember, those are the people who don’t get treatment even though they’re sick. And without that group, it’s kind of hard to say how well a drug works. Most of the remdesivir trials have not had placebo arms, but what’s made a lot of people excited about the positive signal they’re seeing in the NIH trial is it is compared to a placebo, so people who are not getting the drug. And we’re waiting on data from these trials. We just need more information to understand how this is all going to go.
Advertisement
Matt: So we wait and see? I’m picking up on that theme again.
Megha: Yeah, I mean this all takes time. But it’s time we need to take and take now because the experts I spoke with said this virus isn’t going anywhere. And there’s still a lot left to learn about it. You know, I asked a lot of people what they thought this will look like going forward and their answer was, “We don’t know. We need to wait and see. And we need to be cautious.” Here’s Sina Bavari again.
Sina Bavari: We don’t really have a lot of information right now. I just definitely don’t think we are at the tail end of it. Is this going to be a seasonal disease? I don’t know. I’m not sure yet. Until we go through the first couple of seasons, it’s very difficult to say. Is it going to be something that we’re going to have to get used to it for many years? Don’t know. Sorry.
Megha: And Lisa Gralinski from the University of North Carolina had similar thoughts.
Lisa Gralinski: So right now, I don’t have a great deal of hope with the way things are going right now that we’re going to see a significant wane in the Northern Hemisphere during the summer months, just because there’s so much human-to-human transmission going on that we’re nowhere near there having control of this virus.
But even if we do see some wane, right now, there’s so much virus around, there will still be pockets of people, even best-case scenario that are still spreading the virus, so it would be pretty easy for it to surge back.
Hopefully, we can all recognize that this is an extraordinary situation that we should do our best to avoid having to repeat. I think the world has learned some really important lessons about the necessity of surveillance programs and preparation. So I do hope that in the years to follow that we will have a better footing if something like this does happen again, but right now we’re kind of stuck.
Megha: I mean, I don’t want to paint this rosy picture of what’s happening because I don’t think that it’s fair. That being said, there’s a lot of really good work going on, a lot of collaboration. And a lot of industry and academia coming together. And a lot of multinational, multi-company collaborations going on trying to solve this coronavirus problem.
Everyone is working as fast as they can while this infection rages all around us. And regardless of what treatments and vaccines eventually get to market, social distancing and staying at home, Zoom schooling our children, baking new and wilder loaves of bread, again, this is all about buying us time. Because even as fast as researchers can work, as fast as manufacturers can make things, we still don’t know what will work, or frankly, if anything will work.
So what we are trying to do to keep the infection rate and the death rate as low as possible while we build and test all these molecular safeguards. When it comes to COVID-19, we’re what, barely 5 months in? We really have only just begun.
This episode was written by me, Megha Satyanarayana.
Matt: And produced by me, Matt Davenport. Stereo Chemistry is a production of C&EN, the news magazine of the American Chemical Society.
Megha: Our editors are Lisa Jarvis, Lauren Wolf, and Amanda Yarnell. Our copyeditor is Sabrina Ashwell.
Matt: The music you heard in this episode was “Wonder About You” by Itai Argaman, “Listening” by GHST MDRN, “Ambrosial” by Kadir Demir, “Bigend” by Tomer Ben Ari, and “Paradox” by Shahead Mostafafar.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter