Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Drug Discovery
tRNA therapies could help restore proteins lost in translation
A new class of therapies based on transfer RNA could treat forms of cystic fibrosis, muscular dystrophy, genetic epilepsies, and more
by Ryan Cross
September 19, 2021
| A version of this story appeared in
Volume 99, Issue 34

Credit: William Ludwig/C&EN/Science Source
When Daniel Fischer cofounded Tevard Biosciences in 2017, he wasn’t trying to bet on the next hot RNA technology. His interest was more personal. His daughter Natasha has Dravet syndrome, a rare form of epilepsy caused by a genetic glitch in a type of sodium channel. This protein conducts electrical signals that brain cells use to communicate. For years, the glitch tormented Natasha with more than 40 small seizures every night. Fischer and his wife took turns staying up with her. “We didn’t sleep,” he says.
In brief
More than 10% of all genetic diseases are caused by mutations that prevent cells from making fully formed proteins. An experimental therapy that uses suppressor transfer RNA (tRNA) could help overwrite these mutations and restore normal protein production. Although the technique dates back nearly 40 years, biotech companies are finally taking the idea seriously, with tRNA-based therapies in development for cystic fibrosis, Dravet syndrome, Duchenne muscular dystrophy, and Rett syndrome. But to be successful, these therapies will need to overcome drug delivery challenges common to all RNA molecules and safety concerns unique to tRNA.
Several medications have helped reduce the frequency of Natasha’s seizures, but her disease has taken a cognitive and physical toll on her. Fischer has made it his life’s work to find a cure for Dravet. He explored the possibility of using gene therapy or gene editing—technologies that were dominating headlines for their ability to tackle other rare genetic disorders. But scientists told him those approaches would be difficult to implement for Dravet. Instead, a newfangled idea called transfer RNA (tRNA) therapy seemed like it might be the answer.
Transfer RNA, or tRNA, as it’s known to biologists, helps cells assemble proteins from amino acids by translating the nucleotide code of messenger RNA (mRNA). Each tRNA molecule reads a trio of nucleotides called a codon, which represents instructions for adding a particular amino acid to a protein. The tRNA then earns its name by transferring the corresponding amino acid to the cell’s protein-making machinery, known as the ribosome. This process repeats along the length of the mRNA strand until the ribosome runs into a stop codon, a special trio of nucleotides that marks the end of the protein-making instruction manual. The ribosome’s job is done.
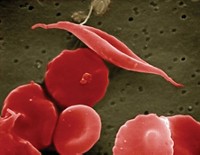
That’s how it’s supposed to work, anyway. But sometimes, genetic mutations can cause typos that change one codon to another, prompting a tRNA to add the wrong amino acid—which leads to proteins that are fully formed but not always properly functioning. More critical errors can occur too. About one in four people with Dravet, including Natasha, has a mutation that creates premature stop codons, like a misplaced period interrupting the middle of a sentence. tRNAs don’t bind to them, and when Natasha’s ribosomes come across these misplaced periods, they mistakenly think they’ve finished making her sodium channels, leaving a mangle of amino acids in their place.
Now, a handful of biotech companies, including the one cofounded by Fischer, are working on treatments called suppressor tRNAs that override premature stop codons like the ones in Natasha’s cells. The idea is to create molecules that bind to those errant codes and deliver the amino acid that is supposed to go in that part of the protein. Doing so should allow Natasha’s ribosomes to finish making the entire sodium channel and correct the balance of electrical signals in her neurons.
Although Fischer’s interest in suppressor tRNA remains deeply personal, his vision for what the technology could achieve has greatly expanded since cofounding Tevard. Premature stop codons are responsible for more than 10% of all genetic diseases, including some types of cystic fibrosis and Duchenne muscular dystrophy. Fischer thinks that if a drug based on suppressor tRNA can quell Natasha’s seizures, the same drug could potentially treat other epilepsies or even different genetic diseases that are caused by the same kind of premature stop codon, regardless of what gene the codon appears in.
Three start-ups—ReCode Therapeutics, Shape Therapeutics, and Tevard—have collectively raised more than $240 million to develop suppressor tRNA therapies. Research grants and patents suggest that other academic and industry groups are beginning to take interest in tRNA as well, partly because of the potential versatility of the technology. “In principle, once we get a tRNA approved for one use, that exact same tRNA could be used for other diseases that also have that same type of mutation,” says David Lockhart, CEO of ReCode Therapeutics. “I told that to one of our investors and their eyes lit up.”
Although promising, suppressor tRNA therapies are no sure thing. Drug delivery is still a challenge for any RNA molecule, and developers will need to prove that their suppressor tRNAs don’t interfere with normal genes and spur ribosomes to produce potentially toxic proteins.
The good news is that these challenges seem more surmountable than ever. Moderna and Pfizer have both proved RNA’s worth with their successful COVID-19 vaccines and the lipid nanoparticle delivery technology they use. “This is a year when all of the sudden our potential to deliver RNA to cells has become clearer,” and tRNA looks like a good one to try, says Rachel Green, a molecular biologist at Johns Hopkins University. “But anyone who studies the ribosome will say, ‘Cool idea. Now show me you can do it.’ ”
Stopped too soon


BLOWING THROUGH STOP SIGNS
The idea of engineering tRNA to treat genetic diseases has been around for almost 40 years—nearly as long as scientists have known about the molecule. But until recently, suppressor tRNA therapies have received little interest from academics and practically no investment from biotech companies. Instead, the industry long fixated on curing genetic diseases by replacing or fixing DNA.
Gene therapy, which uses an engineered virus to deliver a new piece of DNA into someone’s cells, and gene editing, which uses systems like CRISPR to change or replace the existing DNA, are both poised to make enormous strides in the treatment of genetic diseases. But neither technology is a panacea.
Take Dravet as an example. The regulation of SCN1A, the gene that encodes that crucial sodium channel, is tightly controlled. A gene therapy that causes too much of the protein to be made could be just as dangerous as a mutation that makes too little. And even if a gene therapy could strike the proper balance, Fischer says, there is a more immediate obstacle: SCN1A is simply too large to be packaged into the engineered viruses currently used to deliver gene therapy. That packaging problem applies to the errant genes behind many other rare diseases, like cystic fibrosis and muscular dystrophy.
CRISPR gene editing also has the same packaging-size restrictions as gene therapy and carries the risk of making permanent problematic changes to DNA. In 2017, Prashant Mali’s lab at the University of California San Diego published early work describing how suppressor tRNAs and another technology called RNA editing could be a “genomically scarless” alternative to gene editing—a bold claim from a scientist who in 2013 became among the first to test CRISPR on human cells in the lab.
“CRISPR isn’t going to be great for everything,” says David Huss, head of research at Shape Therapeutics, which was formed in 2018 on the basis of Mali’s work. “We need to be more open to finding what works best for each disease.”
As investors have become more attuned to the potential limitations of gene therapy and gene editing, competing technologies that leave DNA and its finely tuned regulation untouched are starting to carve out a niche. “The tRNA approach keeps all that subtlety in the genome intact and just fixes the problem downstream of all that regulation,” says Robert Blazej, a partner at Mission BioCapital, a venture firm that invested in Shape. The start-up is now developing suppressor tRNAs to treat a neurodevelopmental disorder called Rett syndrome, in which about 30% of cases are caused by premature stop codons.
Around the same time that Shape was getting off the ground, four scientists at Texas A&M University and the University of Texas Southwestern Medical Center were developing a suppressor tRNA therapy for forms of cystic fibrosis caused by premature stop codons. Those mutations account for about 10% of cystic fibrosis cases, including the ones that are not treatable with existing small-molecule drugs. The work became the basis of ReCode Therapeutics. “It was an exciting new avenue that no one had ever done before, and it was really out of the box,” says William Skach, chief scientific officer of the Cystic Fibrosis Foundation, which helped fund ReCode. Fischer, meanwhile, was busy cofounding Tevard with Warren Lammert, a private investor whose daughter also has Dravet, and Harvey Lodish, a professor at the Massachusetts Institute of Technology and the Whitehead Institute.
To make their suppressor tRNA therapies, these companies must first understand how normal tRNAs work. The molecules are made from RNA strands that are usually 70 to 80 nucleotides long—bite size compared with the thousands of nucleotides in each mRNA strand in a COVID-19 vaccine. More importantly, while mRNA is an information molecule, tRNA is an action molecule.
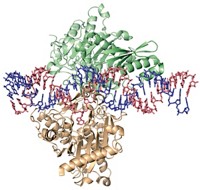
tRNA strands twist into a 3D structure that from a certain angle looks like the state of Florida. When the tRNA’s southern tip, called its anticodon, pairs with the corresponding codon on mRNA, the tRNA’s panhandle transfers an amino acid to the ribosome. The anticodon is the primary site that scientists tinker with when making their suppressor tRNAs. Although tRNAs don’t normally bind to stop codons, scientists can simply change one to three nucleotides in the anticodon to make synthetic versions that do. “They are trivial to make,” Lodish says.
As an example, the codon CGA instructs a tRNA to transfer the amino acid arginine to the ribosome. A common genetic mutation converts CGA to UGA, turning an arginine codon into a premature stop codon. By designing suppressor tRNAs that bind to UGA and transfer an arginine to the ribosome, the companies hope to overwrite the errant stop signal and allow the rest of the protein to be made. “The ribosome keeps chugging along like nothing strange happened,” Shape Therapeutics’ Huss says.
Our bodies have hundreds of different tRNAs, each dedicated to transferring one of the 20 amino acids used to build proteins in humans. Why, exactly, we need so many tRNAs is still somewhat of a mystery, but it gives suppressor tRNA developers a lot of territory to explore. In 2019, Christopher Ahern at the University of Iowa and one of his former postdoctoral researchers, John Lueck, published results from a study that used those natural tRNAs as the foundation for designing and testing hundreds of suppressor tRNAs. “There were a lot of losers, and also some winners for each tRNA family,” says Lueck, who is now working on the approach in his own lab at the University of Rochester Medical Center.
Tevard licensed the academic team’s suppressor tRNAs and tested a promising one in cells containing Natasha’s premature stop codon. “Without a suppressor tRNA, there is nothing made,” Lodish says. “If you add the suppressor tRNA, you get a full-length protein.” More importantly, electrical readings of the cells show that the resulting sodium channels open and close as if there was never a mutation to begin with. “It is perfectly normal,” Lodish says.
That same suppressor tRNA could be used for other applications too. “Any arginine-to-UGA mutation can be reversed by these tRNAs,” Lodish says. This is a key selling point for companies developing suppressor tRNAs: unlike gene therapy and gene editing, which have to be designed with a specific gene and specific disease in mind, tRNA therapies could work for many people with diseases caused by the same kind of premature stop codon.
Advertisement
The arginine-to-UGA switch, along with two other mutations, accounts for nearly half of all known diseases caused by premature stop codons. Tevard is combining suppressor tRNAs for all three into a single therapy dubbed Tristop, which it thinks could treat at least two-thirds of all Duchenne muscular dystrophy cases caused by premature stop codons. The combination approach would make it easier to design a single therapy that can be used in a wide range of patients, but the strategy also raises the risk of side effects. The company is testing Tristop in mice with Duchenne now and is talking to larger companies that focus on muscular dystrophy about partnering on the technology.
Tevard is also in the early stages of developing a completely different strategy that it calls enhancer tRNA therapy. While suppressor tRNAs are designed to restore protein production from faulty genes, enhancer tRNA therapies could help double protein production in people who have a class of disease driven by mutations that allow them to make only half the protein they need, explains Jeff Coller, an RNA scientist at Johns Hopkins who helped test the approach. Tevard is partnering with the epilepsy drug company Zogenix to study both suppressor and enhancer tRNAs for Dravet and other epilepsies.
CHALLENGES OF TRANSLATION
The potential advantages of suppressor tRNA therapies hinge on two strongly held beliefs by the companies developing them: first, that these synthetic molecules will be safe, and second, that scientists will be able to deliver them into the body using some of the same technologies that gene therapies and mRNA vaccines are based on. Neither is a given.
The question of safety has long been an intellectual barrier to developing suppressor tRNAs. Scientists aren’t sure if suppressor tRNAs will pair only with their intended targets—those premature stop codons—or if they might also bind to normal stop codons. After all, the UGA sequence found in a premature stop codon in Dravet syndrome is made of the same three nucleotides found in normal stop codons in thousands of other mRNAs. The result could be gobbledygook sequences of amino acids appended onto the ends of otherwise normal proteins.
“One would expect the suppressor tRNA to really screw up the cell,” says Arthur Johnson, a cofounder of ReCode and an emeritus professor from Texas A&M. “But that is not what happens.”

A technique called ribosome profiling helps explain why. The method allows scientists to take a snapshot of the thousands of ribosomes that at any given time are scooting along mRNA strands and making proteins in our cells. Scientists freeze the ribosomes in their tracks, degrade all the mRNA that the ribosomes are not actively reading, and then separate and sequence the small fragments of mRNA left behind. The result gives scientists an idea of what the ribosomes are reading and whether they are mistakenly scooting past stop codons, Rochester’s Lueck says.
Experiments in normal cells show that mistakes are somewhat common. Ribosomes may inappropriately read past a stop codon up to about 1% of the time. Ahern and Lueck partnered with scientists at the Cystic Fibrosis Foundation to run a ribosome-profiling study of their suppressor tRNAs. In general, the team found that most of their molecules didn’t cause much more ignoring of stop codons than normal. “That was one of the most surprising, useful, and serendipitous results that we came across,” Ahern says, calling it “one of the mysteries” of the technology. It’s also a crucial selling point. “These biotech companies would probably have never wanted to touch it without that data,” he says.
Scientists readily admit that they don’t fully understand why suppressor tRNAs seem to favor premature stop codons. But they think that the context of a normal stop codon and not simply its specific trio of nucleotides matters. Normal stop codons, and the mRNA sequences around them, attract molecules that help wind down translation, Ahern says. And in the instances where the ribosome does sneak past a normal stop codon, our cells have fallback systems for degrading the resulting proteins.
Those fallback systems do not mean companies can guarantee the safety of suppressor tRNAs. Only clinical trials can prove that. And Johns Hopkins’s Green, whose lab specializes in studying translation, says it is possible that the molecules could trigger ribosomes to read past stop codons on mRNA strands that ribosome-profiling experiments are not capable of detecting.
A bit of tRNA engineering could help alleviate some of the safety concerns. Zoya Ignatova, a tRNA scientist at the University of Hamburg, says she has changed the size of the tRNA anticodon loop to make the molecules preferentially bind to premature stop codons over regular stop codons. Her pending patent on the technology is assigned to the mRNA therapy company Arcturus Therapeutics. She thinks that tinkering with other parts of tRNA’s structure could help make the molecules better drugs too.
Safety isn’t the only unknown for the tRNA field. When investors ask ReCode’s Lockhart why no one has tried to develop suppressor tRNA therapies before, he points to delivery. Anyone can get the molecules to work in a petri dish, Lockhart says, but getting sufficient amounts of functional tRNA into the body is another matter entirely. Companies are focused on two approaches to solving this delivery problem: packaging synthetic tRNA molecules in lipid nanoparticles or encoding genetic instructions for making tRNA in an engineered virus such as an adeno-associated virus (AAV).
Shape and Tevard are both using AAVs to deliver genes for their suppressor tRNAs into cells, an approach that essentially creates a one-and-done gene therapy. When the virus enters a person’s cells, a strand of DNA encoding instructions for making the suppressor tRNAs will endow them with the ability to maintain a steady, potentially permanent supply of those tRNAs.
ReCode, meanwhile, is using technology from UT Southwestern chemist Daniel Siegwart to package its chemically synthesized tRNAs into proprietary lipid nanoparticles. “Doses can be adjusted, stopped, and spaced. You have better control over your drug,” than with AAVs, Lockhart says.
“Both systems have pros and cons,” Ignatova says, adding that the best system may depend on where, exactly, the companies want to deliver their tRNA.
A third unknown for the tRNA field is whether the nascent technology will be crowded out by existing approaches or others yet to come. Shape, for instance, is developing an RNA-editing technology to correct mutations in mRNA. ReCode is developing mRNA therapies to replace the broken gene in cystic fibrosis, which the firm thinks it can deliver with lipid nanoparticles. After recently comparing ReCode’s suppressor tRNA and mRNA approaches head to head, Lockhart says that ReCode will prioritize the mRNA therapy for cystic fibrosis.
The Cystic Fibrosis Foundation wants to keep both technologies, and others, such as gene editing, on the table. “In the end you never know which approach is going to win, and it is probably better to pursue multiple approaches,” Skach says.
Even if an approach is feasible, that doesn’t mean it is practical. For instance, a form of CRISPR called base editing can fix single-nucleotide mutations in DNA, but that approach requires the therapy to be customized for each unique mutation, including the same nucleotide switch that can appear in different spots in the gene. “We could do it for Natasha, but it won’t be generalizable,” Fischer says. Although he acknowledges that suppressor tRNA won’t work for everything, he thinks it is still the best option for diseases caused by mutations in large genes that require finely tuned regulation. “That’s where we really have a competitive advantage against other approaches.”
“Our initial goal was to cure Dravet,” Fischer says. Now his firm is looking to expand its tRNA work into additional kinds of epilepsies and eventually into neurodegenerative and psychiatric disorders. Academic scientists have plans to develop suppressor tRNAs for genetic forms of blindness, a lysosomal storage disease called Hurler syndrome, and even a form of autism caused by mutations in a sodium channel.
Natasha, now 12, has fewer seizures than before, but she has developed problems walking and controlling her behavior. “The big issue right now is quality of life” for her and her family, Fischer says. Something that helps her be a bit more independent would be a godsend, he adds. Once Tevard finishes preclinical studies of its suppressor tRNA therapy for Dravet, its partner, Zogenix, will be responsible for the clinical trial. He can’t say when, exactly, it will start. “Hopefully soon.”



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter