Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Drug Discovery
Drug structures displayed for the first time in Orlando
One reporter’s play-by-play of 8 talks that unveiled potential drugs for cancer, diabetes, bacterial infections, and Parkinson’s disease
by Tien Nguyen
April 5, 2019
As the American Chemical Society national meeting in Orlando wound down, medicinal chemists flocked to a convention center ballroom to hear the stories of eight potential drugs at the start of their likely years-long journey through the clinic to one day reach patients—or so drugmakers hope. An always highly anticipated session, the “First-time Disclosure of Clinical Candidates,” put on by the Division of Medicinal Chemistry, rewards curious chemists with glimpses of drug-candidate structures not previously made public. This year’s session was organized by Erin DiMauro, Merck & Co.’s executive director of discovery chemistry. Half of the talks in the lineup revealed compounds in the recently revitalized area of immuno-oncology that enlist humans’ immune systems to combat tumors. Other presenters shared drug-development programs tackling diabetes, resistant bacterial infections, acute myeloid Leukemia, and Parkinson’s disease.
Candidate: AB680

Presenter: Kenneth V. Lawson, senior scientist at Arcus Biosciences
Target: Ecto-5’-nucleotidase (CD73)
Disease: Cancer
Reporter’s notes: In the first talk of the day, Lawson introduced the idea of cancer drugs that target the host’s immune system. “Checkpoint inhibitors changed the way we think of treating cancer,” he said. These drugs successfully disrupt the binding interaction between a protein and a checkpoint protein that stops immune T cells from killing cancer cells. As a result, these drugs turn immune cells loose to attack tumor cells. But the drugs work only in about 30-40% of patients—an issue pharmaceutical companies like Arcus hope to address with new immunotherapies that can be taken in combination with checkpoint inhibitors.
Lawson’s team set out to inhibit an enzyme commonly found in tumors called CD73, the second of two enzymes which break down extracellular adenosine trisphosphate (ATP) to adenosine. Adenosine then binds to immunosuppressive receptors on immune cells and shuts them down. Yet developing a small molecule inhibitor of CD73 proved challenging, Lawson said. After striking out with high-throughput screening, the team turned to CD73’s natural substrate for inspiration. However, the molecule possessed more than one phosphate group, which is notoriously a liability for drug molecules because small molecules with such negative changes struggle to cross cell membranes. The team’s goal was to remove the phosphate groups, Lawson says, but things didn’t exactly go according to plan. After showing the audience a series of compounds from structure-activity relationship (SAR) studies—slides no medicinal chemistry talk would be complete without—Lawson revealed the structure of their final clinical compound AB680 as the sound of people flipping notebook sheets rippled across the room. Synthesized in 34% overall yield, the candidate ultimately included two phosphate groups—a feature that surprised audience members.
Tests revealed that AB680 can be given intravenously but the compound also showed moderate oral bioavailability. Lawson suggested a possible route for how the molecule might pass from the digestive tract to the bloodstream, a paracellular mechanism by which molecules cross the epithelium by passing through the space between cells. AB680 showed “extraordinary potency,” inhibiting CD73 in human T-cells at a concentration of 0.008 nM. The compound has a 4 day half-life, which means it could be dosed every two weeks, coinciding with the dosing schedule for patients who receive a checkpoint inhibitor. AB680 is currently in Phase 1 clinical trials with healthy patients.
Candidate: LHC165

Presenter: Alex Cortez, senior Investigator I at the Genomics Institute of the Novartis Research Foundation
Target: Toll-like receptor 7 (TLR7)
Disease: Solid tumors
Reporter’s notes: Cortez shared another story in the realm of immuno-oncology, although the program that yielded this compound actually started in the world of vaccines. Cortez’s team had been focusing on vaccine adjuvants, small molecules that turn on the immune system to enhance a vaccine’s effect. They developed one such class of compound that activates toll-like receptor 7 (TLR7), a protein in the immune system that recognizes dangerous-looking molecules and can trigger the release of infection-clearing proteins. After observing TLR7 agonists’ ability to induce an immune response with vaccines, the researchers wondered whether the molecules could also be effective in immuno-oncology.
They found that LHC165 adsorbed to aluminum hydroxide reduced tumor growth in mice and, intriguingly, showed signs of an abscopal effect, in which untreated tumors shrink concurrently with treated tumors. The implication is that if the immune system recognizes one tumor site, it can recognize others. As with several of the candidates presented throughout the day, LHC165 bears a phosphate group and is injected into the tumor. It’s currently in Phase I trials in patients with advanced malignancies, which means they’ve already tried second and third line therapies, as a single agent and in combination with the checkpoint inhibitor PDR001.
Candidate: VNRX-7145

Presenter: Christopher John Burns, president and chief executive officer of VenatoRx Pharmaceuticals
Target: β-lactamases
Disease: Resistant urinary tract infections
Reporter’s notes: Having unveiled an antibacterial candidate at last spring’s first time disclosures session, Burns was back with another, this time the molecule can be taken orally. Both VenatoRx (pronounced Ven-a-tor-ix) compounds resuscitate the activity of β-lactam drugs, which make up more than 60% of all antibiotics prescribed. Unfortunately, many bacteria have grown resistant to these antibiotics. The new compounds rescue the old antibacterials by inhibiting β-lactamases, enzymes that chew up the antibiotics. To test the activity of new β-lactamase-targeting compounds, the researchers settled on several “sentinel” bacteria strains. Then to find a candidate with oral bioavailability, the team focused on molecules with low polarity and low molecular weight. They found VNRX-7145, developed as a prodrug in which esterases in the liver clip off the tips of the molecule to reveal the active drug. VNRX-5133, disclosed at last year’s meeting, had to be delivered intravenously along with another IV-antibiotic Cefepime, and targeted serine and metallo β-lactamases. The new oral candidate VNRX-7145 inhibits serine β-lactamases with Ceftibuten as its partner. The VNRX-7145 combination is now in Phase I studies to treat resistant urinary tract infections.
Candidate: TAK-981

Presenter: Steven Paul Langston, associate director at Takeda Pharmaceuticals International
Target: Sumo activating enzyme
Disease: Solid tumors
Reporter’s notes: Langston gave the last talk of the morning session, placing him in the “precarious position of being between you and lunch,” he said. Takeda acquired this drug development program, falling under the umbrella of immuno-oncology, along with Millenium Pharmaceuticals in 2008. The team targeted a pathway known as SUMOylation, a protein post translation modification that is implicated in a number of cellular processes including immune response. In SUMOylation, enzymes attach a small protein to another protein. They found that inhibiting this pathway activates a type I interferon response in immune cells. How the molecule, TAK-981, inhibits this pathway is quite complicated, Langston said. TAK-981 forms an adduct with a small ubiquitin like modifier (SUMO) to inhibit a SUMO activating enzyme that catalyzes SUMOylation. While the synthesis of TAK-981 is fairly short, it requires a nonideal chiral chromatography separation after the first step. TAK-981 is in Phase I clinical trials as an intravenous infusion for patients with metastatic solid tumors or lymphomas.
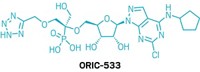
Candidate: AMG 510

Presenter: Victor Cee, research director at Amgen
Target: Kirsten rat sarcoma viral oncogene homolog position G12C (KRas G12C)
Disease: Solid tumors
Reporter’s notes: After lunch, Amgen’s Cee kicked off the afternoon session with the disclosure of the much buzzed about first-in-clinic inhibitor of a common mutated protein in solid tumors called KRas G12C, which was discovered decades ago. “We’ve known about it for a long time but haven’t been able to do anything about it,” Cee said. At least, not until now. KRas has an off state, which binds to guanosine diphosphate, and an on state, which binds to guanosine triphosphate. Medicinal chemists have viewed the on state as impenetrable, Cee said. To make the point, he displayed its protein structure next to an image of the Death Star from Star Wars, drawing chuckles from the crowd. But, he said, like the Death Star, the active form of the KRas G12C mutant has a fatal engineering flaw: It has a cysteine mutation that molecules can attach to. This cysteine is even more vulnerable in the off state, which the researchers could target since the protein switches rapidly between both states.
The team advanced a series of promising compounds that were ultimately abandoned due to poor stability. Then they introduced what Cee called a “magic isopropyl group,” giving them a molecule with improved stability and ability to inhibit KRas G12C. But the resulting molecule was an atropisomer, a molecule that can rotate from one distinct chiral form to another with a half-life of 8 days, a featue that would raise a red flag for most in the industry. The team could either try to modify their molecule to eliminate its chirality or increase the barrier to rotation to slow down the isomerization and trap it in one form. They went for the latter option and found that adding a methyl group led to a half-life of more than 2,000 years. Still, the lead molecule wasn’t very soluble, which would have meant the drug couldn’t be taken orally, but two more heteroatom switches finally led the scientists to a compound with desirable properties—AMG510. Currently, the compound is being tested in Phase I clinical trials in patients with advanced KRas G12C solid tumors. Read our full story here.
Candidate: ABBV-951

Presenter: Philip Kym, director of chemistry at AbbVie
Target: Dopamine receptor
Disease: Parkinson’s disease
Reporter’s notes: Right at the start, Kym told the audience that his talk would be different from the rest in the series. That’s because the AbbVie researchers’ goal wasn’t to discover a new drug, but to try to improve an existing drug: Levodopa. The drug was discovered about 50 years ago and remains the gold standard treatment for Parkinson’s disease, he said. People with Parkinson’s disease are increasingly unable to produce the neurotransmitter dopamine. This dopamine deficit leads to impaired movement. Enzymes in the brain turn Levodopa into dopamine, but the drug has to be dosed with another compound called carbidopa to prevent Levodopa from transforming before it crosses the blood-brain barrier. While Levodopa works well at first, eventually the body becomes dependent on it and its absorption becomes hard to predict.
AbbVie previously developed a way to continuously infuse Levodopa and carbidopa through the intestines to address these issues, but installing the device requires invasive surgery. The company wanted to find a formulation that could be delivered in a less invasive, subcutaneous route, much like how an insulin pump works for people with diabetes. This led the team to incorporate phosphate groups on levodopa, which required a tedious synthesis. The route started with a ~3% overall yield and then the team improved the synthesis to get a 54% yield. Ultimately the team moved forward with ABBV-951, a combination of monophosphate Levodopa and monophosphate carbidopa, which was well-tolerated in rats. The combo is currently in Phase I trials as a 24- and 72-hour subcutaneous infusion in Parkinson’s patients.
Candidate: S64315

Presenter: Andras Kotschy, managing director at Sevier Research Institute of Medicinal Chemistry
Target: Myeloid cell leukemia-1 (MCL-1)
Disease: Acute myeloid leukemia and myelodysplastic syndrome
Advertisement
Reporter’s notes: If a cell wants to commit suicide, it calls on various proteins that help regulate programmed cell death, also called apoptosis, Kotschy said. Cancer cells, however, dodge death by overexpressing antiapoptosis proteins like MCL-1. Scientists have thought about inhibiting MCL-1 as a strategy to kill cancer cells since the 1980s but have struggled to design a drug that can target the protein’s surface. Even a decade ago, researchers were split on the viability of MCL-1 as a target, with the biggest worry that treatments would hit normal cells as well. Today, Kotschy said the risk of toxicity is considered more managable as multiple drug companies, including Servier in collaboration with Novartis, have advanced MCL-1 inhibitors into the clinic. The team has developed S64315 as a single atropisomer now in Phase I clinical trials administered intraveneously in patients with haematological cancers.
Candidate: PF-06882961

Presenter: David J. Edmonds, senior principal scientist at Pfizer
Target: Glucagon-like peptide-1 (GLP-1) receptor
Disease: Diabetes
Reporter’s notes: Finishing out the session, Pfizer’s Edmonds presented a compound joining a growing and lucrative class of molecules targeting the GLP-1 receptor for the treatment of diabetes and obesity. GLP-1 is a 30 amino acid peptide hormone that triggers insulin secretion in pancreatic cells. Its receptor has proven difficult to activate with small molecules. Existing molecules that can turn on the receptor are peptides delivered by injection, Edmonds said, making the case for designing a molecule that could be taken orally. Following a screen of Pfizer’s library of 2.8 million compounds, the researchers conducted a series of studies, taking a “brute force” approach that looked solely at activity. Eventually, the team landed on PF-06882961, which has completed Phase I trials in healthy adults.



Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter