Infectious Disease
Coronavirus research dominated 2020
SARS-CoV-2 went from a mysterious new virus to the subject of thousands of papers in a year
by Laura Howes
One topic has dominated much of the scientific literature this year, just as it has dominated news reports and family conversations: the novel coronavirus and COVID-19, the disease it causes. Cases of the pneumonia-like disease were reported in December 2019, but the coronavirus, now known as SARS-CoV-2, became the story of 2020.
Using computational methods, the COVID-19 Dispersed Volunteer Research Network recently analyzed the scientific literature for publications related to COVID-19. It found thousands. Anhvinh Doanvo, the data scientist who led the project, tells C&EN that group members analyzed the scope of coronavirus research performed this year (Patterns 2020, DOI: 10.1016/j.patter.2020.100123). They found that most publications focused on public health, outbreak reporting, clinical care, and testing for coronaviruses. A smaller number focused on basic research. But, Doanvo says, “there’s a massive amount of effort being devoted to every area in basic science” to study this virus. Here’s a look at some of 2020’s coronavirus research.
Structures
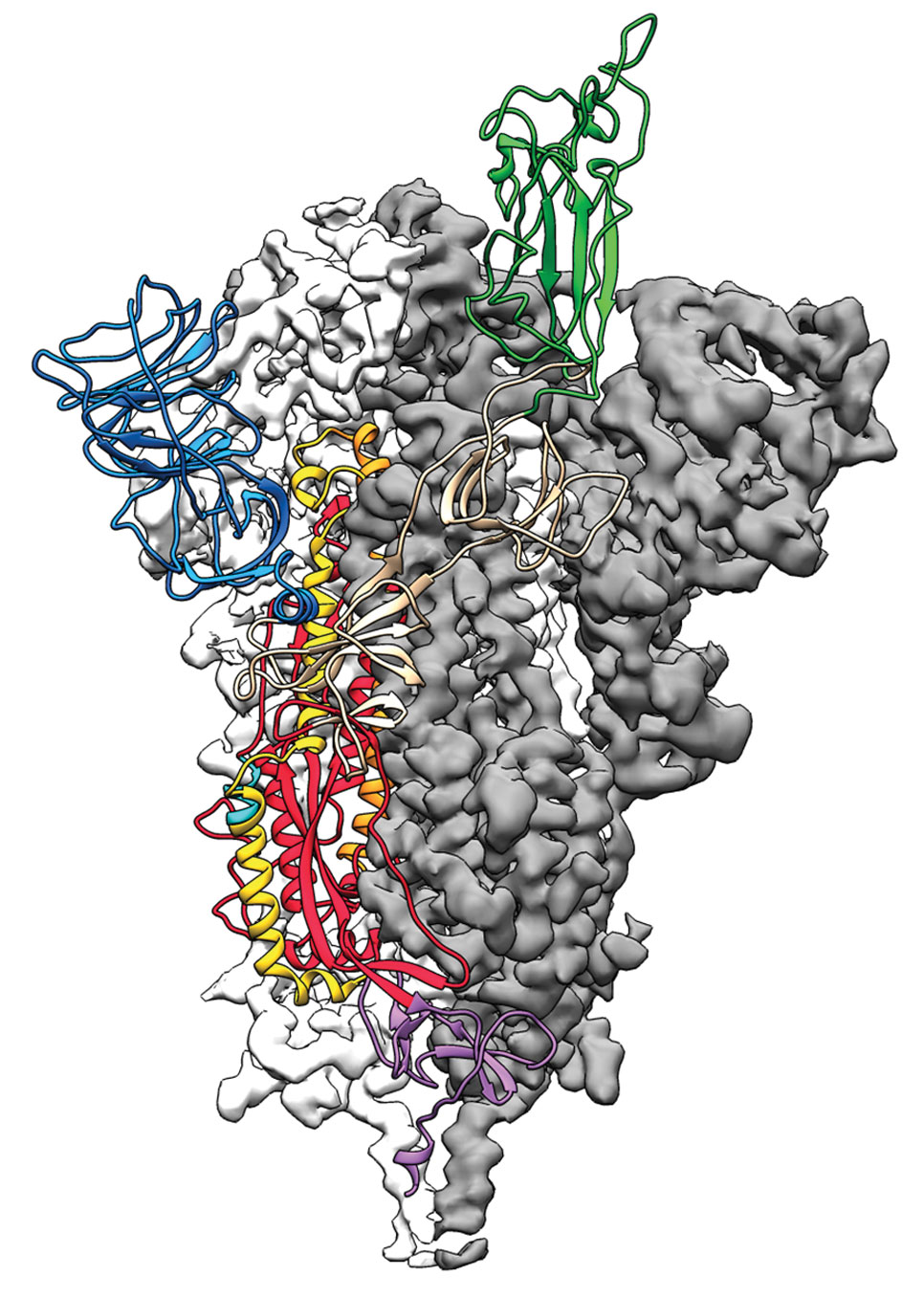
After SARS-CoV-2’s genetic code was published Jan. 10, structural biologists jumped into action to understand the 3-D structures of the virus’s proteins. Their aim was to know not just how the virus works on a molecular level but also how to guide the design of drugs, vaccines, and antibody therapies. The virus’s spike protein, a segment that latches onto and infects human cells, has now been imaged multiple times. It took just a couple of weeks for Jason McLellan and coworkers at the University of Texas at Austin to determine the initial structure (Science 2020, DOI: 10.1126/science.abb2507). Since then, other teams have imaged drugs bound to the virus’s main protease and its RNA-dependent RNA polymerase (Science 2020, DOI: 10.1126/science.abb3405 and 10.1126/science.abb7498), as well as antibodies bound to the spike protein (Science 2020, DOI: 10.1126/science.abb7269). In fact, by late November, an international repository of biological structures known as the Protein Data Bank contained data for over 500 coronavirus-related structures. But the work isn’t finished. Researchers continue to screen for drug candidates and antibody therapies and solve the structures of more viral proteins (Nat. Struct. Mol. Biol. 2020, DOI: 10.1038/s41594-020-00536-8).
Masks

As the COVID-19 pandemic began to unfold, people in Asian countries were quick to don masks to stop the virus’s spread, but people elsewhere were slower. Public health officials in Europe and the US decided they did not know enough about the way SARS-CoV-2 spread and were concerned that encouraging people to buy masks could lead to shortages for health-care workers. Within a few months, however, observational studies and lab tests presented a body of evidence indicating that masks help slow the spread of the disease (Morb. Mortal. Wkly. Rep. 2020, DOI: 10.15585/mmwr.mm6928e2 and 10.15585/mmwr.mm6931e1). The US Centers for Disease Control and Prevention now says masks reduce the number of virus-containing droplets people release when they exhale and may also minimize droplet inhalation. To help shoppers and do-it-yourself types find or sew the most effective reusable mask, scientists at the University of Chicago and Argonne National Laboratory sought to identify the best fabric to use. They showed that layers of tightly woven cotton or silk and mixtures of materials are good choices (ACS Nano 2020, DOI: 10.1021/acsnano.0c03252 and 10.1021/acsnano.0c04897). Stanford University materials scientists showed that adding disposable filters made from facial tissues inside homemade masks gives even better results (Nano Lett. 2020, DOI: 10.1021/acs.nanolett.0c02211). Just as with socks and underwear, after wearing a cloth mask, people need to wash it before wearing it again. One study found infectious virus on the outer layer of a surgical mask 7 days after it was worn (Lancet Microbe 2020, DOI: 10.1016/S2666-5247(20)30003-3).
False starts

Our understanding of how the new coronavirus spreads and can be treated and who is most susceptible to infection has changed over the past year. Early public health advice focused on reducing transmission of the virus on surfaces and objects, known as fomites, but the importance of surface transmission was soon contested, and research began to focus on airborne transmission. Doctors have long known that viruses hitch a ride on large droplets of spittle that fall quickly to the ground. But the idea that smaller droplets could spread the disease as they waft in the air was controversial. Nevertheless, air measurements in hospitals in Wuhan, China (Nature 2020, DOI: 10.1038/s41586-020-2271-3), and outdoors in Northern Italy (Environ. Res. 2020, DOI: 10.1016/j.envres.2020.109754), among other places, implicated aerosols as a potential infection risk.

Meanwhile, another idea that was debated in the scientific literature was whether having type O blood protected people from the severity of COVID-19. Multiple studies of patients hinted that people with type A blood had a higher chance of developing severe respiratory failure compared with people with type O blood; some of these studies were published in preprint servers and thus haven’t been peer-reviewed (medRxiv 2020, DOI: 10.1101/2020.05.31.20114991, 10.1101/2020.03.11.20031096, and 10.1101/2020.04.08.20058073; Br. J. Haematol. 2020, DOI: 10.1111/bjh.16797). But later studies found no link between blood type and disease severity (Transfusion 2020, DOI: 10.1111/trf.15946; Ann. Hematol. 2020, DOI: 10.1007/s00277-020-04169-1). The authors of one of the later studies, which followed 957 patients admitted to Massachusetts General Hospital with COVID-19, suggested the authors of the earlier studies had not compared their patients with appropriate control groups.







Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter