Advertisement
Grab your lab coat. Let's get started
Welcome!
Welcome!
Create an account below to get 6 C&EN articles per month, receive newsletters and more - all free.
It seems this is your first time logging in online. Please enter the following information to continue.
As an ACS member you automatically get access to this site. All we need is few more details to create your reading experience.
Not you? Sign in with a different account.
Not you? Sign in with a different account.
ERROR 1
ERROR 1
ERROR 2
ERROR 2
ERROR 2
ERROR 2
ERROR 2
Password and Confirm password must match.
If you have an ACS member number, please enter it here so we can link this account to your membership. (optional)
ERROR 2
ACS values your privacy. By submitting your information, you are gaining access to C&EN and subscribing to our weekly newsletter. We use the information you provide to make your reading experience better, and we will never sell your data to third party members.
Oncology
Lingyin Li
Multidisciplinary maven is harnessing the immune system to fight cancer
by Laura Howes
August 14, 2020
| A version of this story appeared in
Volume 98, Issue 31

Credit: Lingyin Li/Stanford (Li); SPL/Science Source (cancer cell);
When chemist Lingyin Li moved to Tim Mitchison’s lab at Harvard Medical School in 2010 for her postdoctoral studies, she wanted to learn some biology. What she didn’t want was to get stuck on a project that was going nowhere. So when Mitchison suggested she look at why a drug called DMXAA had cured cancer in mice but showed no effect in multiple studies in people with lung cancer, she pushed back. In fact, she says, she spent longer fighting Mitchison’s suggestion than she did figuring out why the drug had failed.
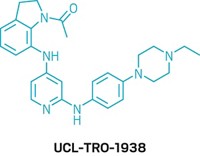
DMXAA, which the big pharma firm Novartis had tested in many cancer trials, was purported to target the stimulator of interferon genes (STING) pathway.
Advertisement
STING is part of the body’s innate immune system—the body’s generalist, first line of defense response to infections. When activated, STING ramps up inflammation. The inflammatory proteins activated by STING then start the more specialized adaptive immune system, with its specific cells and processes. Together, these two parts of the immune system work to eliminate pathogens, and drug companies hoped they could also be used to fight cancer.
Within a few months, Li found that DMXAA binds mouse, but not human, STING. It was the drug, not the target, that was the problem, and researchers went back to find new molecules.

In Mitchison’s lab, Li began to piece together the complex workings of a signaling molecule called cyclic guanosine monophosphate–adenosine monophosphate (cGAMP). Although cGAMP is made inside cells for the express purpose of activating STING, it rather curiously is broken apart by an enzyme found outside cells.
Scientists waved away that enzymatic mystery, but Li wondered if it was something more. Could this signaling molecule have a role outside of cells? She took that puzzle with her when she moved to Stanford in 2015 to set up her own lab.
Since then, Li’s lab has focused on pulling apart this complex part of innate immunity. She’s exploring the molecular details of cGAMP’s relationship with STING and probing where and how it travels in and out of cells. Now, that work is paying off. Li’s lab has a growing body of research demonstrating that extracellular cGAMP is real.
“She took, I thought, a rather risky line of research and seems to be making a lot of progress with it,” Mitchison says, noting the storm of publications coming from Li’s lab.
Earlier this year, Li showed that while cGAMP is continually created inside stressed cells, it doesn’t just stay there. A specific transporter pulls the signaling molecule out of cancer cells. The enzyme Li found during her postdoc, ENPP1, usually then breaks down cGAMP. But if that enzyme is blocked, levels of the signaling molecule rise and then spread to neighboring cells, in turn ringing the alarm for the immune system. Li thinks that inhibiting that enzyme could be exploited as a cancer treatment.
Li’s tenacity when it came to nailing down cGAMP’s role in innate immunity reflects the focus and drive that has characterized her life and her career. Li got into a competitive undergraduate program at the University of Science and Technology of China and went on to earn her PhD with Laura Kiessling at the University of Wisconsin–Madison. When she was diagnosed with breast cancer during her postdoc, that didn’t stop her either. But Li also says she would not have got where she is today without mentorship and support—firstly from her family back in China and later also from scientific mentors and advisers. “Now I’m where I am,” she says, “and I realized, all these people paved the way.”
Vitals
Current affiliation: Stanford University
Age: 39
PhD alma mater: University of Wisconsin–Madison
Hometown: Xi’an, China
If I weren’t a chemist, I’d be: A mathematician. “I am glad I am a chemist hoping to make medicine because, as a mathematician, I would have felt more nonessential in 2020.”
If I were an element, I’d be: Magnesium. “In Chinese, it sounds like the word beautiful. It is not as inflammable as sodium, but when it burns, it lasts longer and gives out the brightest flames.”
When chemist Lingyin Li moved to Tim Mitchison’s lab at Harvard Medical School in 2010 for her postdoctoral studies, she wanted to learn some biology. What she didn’t want was to get stuck on a project that was going nowhere. So when Mitchison suggested she look at why a drug called DMXAA had cured cancer in mice but showed no effect in multiple studies in people with lung cancer, she pushed back. In fact, she says, she spent longer fighting Mitchison’s suggestion than she did figuring out why the drug had failed.
Vitals
▸ Current affiliation: Stanford University
▸ Age: 39
▸ PhD alma mater: University of Wisconsin–Madison
▸ Hometown: Xi’an, China
▸ If I weren’t a chemist, I’d be: A mathematician. “I am glad I am a chemist hoping to make medicine because, as a mathematician, I would have felt more nonessential in 2020.”
▸ If I were an element, I’d be: Magnesium. “In Chinese, it sounds like the word beautiful. It is not as inflammable as sodium, but when it burns, it lasts longer and gives out the brightest flames.”
DMXAA, which the big pharma firm Novartis had tested in many cancer trials, was purported to target the stimulator of interferon genes (STING) pathway.
STING is part of the body’s innate immune system—the body’s generalist, first line of defense response to infections. When activated, STING ramps up inflammation. The inflammatory proteins activated by STING then start the more specialized adaptive immune system, with its specific cells and processes. Together, these two parts of the immune system work to eliminate pathogens, and drug companies hoped they could also be used to fight cancer.
Within a few months, Li found that DMXAA binds mouse, but not human, STING. It was the drug, not the target, that was the problem, and researchers went back to find new molecules.
In Mitchison’s lab, Li began to piece together the complex workings of a signaling molecule called cyclic guanosine monophosphate–adenosine monophosphate (cGAMP). Although cGAMP is made inside cells for the express purpose of activating STING, it rather curiously is broken apart by an enzyme found outside cells.
Scientists waved away that enzymatic mystery, but Li wondered if it was something more. Could this signaling molecule have a role outside of cells? She took that puzzle with her when she moved to Stanford in 2015 to set up her own lab.
Since then, Li’s lab has focused on pulling apart this complex part of innate immunity. She’s exploring the molecular details of cGAMP’s relationship with STING and probing where and how it travels in and out of cells. Now, that work is paying off. Li’s lab has a growing body of research demonstrating that extracellular cGAMP is real.
“She took, I thought, a rather risky line of research and seems to be making a lot of progress with it,” Mitchison says, noting the storm of publications coming from Li’s lab.
Earlier this year, Li showed that while cGAMP is continually created inside stressed cells, it doesn’t just stay there. A specific transporter pulls the signaling molecule out of cancer cells. The enzyme Li found during her postdoc, ENPP1, usually then breaks down cGAMP. But if that enzyme is blocked, levels of the signaling molecule rise and then spread to neighboring cells, in turn ringing the alarm for the immune system. Li thinks that inhibiting that enzyme could be exploited as a cancer treatment.
Li’s tenacity when it came to nailing down cGAMP’s role in innate immunity reflects the focus and drive that has characterized her life and her career. Li got into a competitive undergraduate program at the University of Science and Technology of China and went on to earn her PhD with Laura Kiessling at the University of Wisconsin–Madison. When she was diagnosed with breast cancer during her postdoc, that didn’t stop her either. But Li also says she would not have got where she is today without mentorship and support—firstly from her family back in China and later also from scientific mentors and advisers. “Now I’m where I am,” she says, “and I realized, all these people paved the way.”

















Join the conversation
Contact the reporter
Submit a Letter to the Editor for publication
Engage with us on Twitter